Telehealth vs. Telemedicine: Getting to Know the Nuances

In the rapidly expanding realm of digital healthcare, professionals and patients alike can sometimes find themselves lost in a maze of terminologies. Among the most interchanged – and often misinterpreted – terms are telehealth vs. telemedicine.
Distinguishing between these two is essential not just for accuracy’s sake but for understanding the broader possibilities and specific applications of digital health. So, if terms like telemedicine vs. telehealth leave you baffled or seeking a deeper understanding, you’re on the right track. Here, we aim to explain these concepts, shedding light on their distinct roles in the digital health arena.
from 25 countries outsourced software development to Relevant
We provide companies with senior tech talent and product development expertise to build world-class software.
What is Telehealth?
Imagine a typical weekday evening in a suburban community. As a parent, you’re confronted with your child’s unexpected fever. The closest hospital is miles away, and the neighborhood clinic is shut. In such moments, the immense value of Telehealth becomes evident.
Telehealth leverages the digital domain to facilitate health services, from consultations to certain treatments, minus the constraint of geographical distance. It’s the intersection of healthcare’s commitment with today’s technological advancements, sounding the thought, “Regardless of your location, we’re available.”
Utilizing platforms from interactive video sessions to instantaneous data-sharing mechanisms, Telehealth extends its arms to patients everywhere. Whether you’re in a bustling city or a serene village, Telehealth ensures everyone has equal access to top-tier medical assistance.
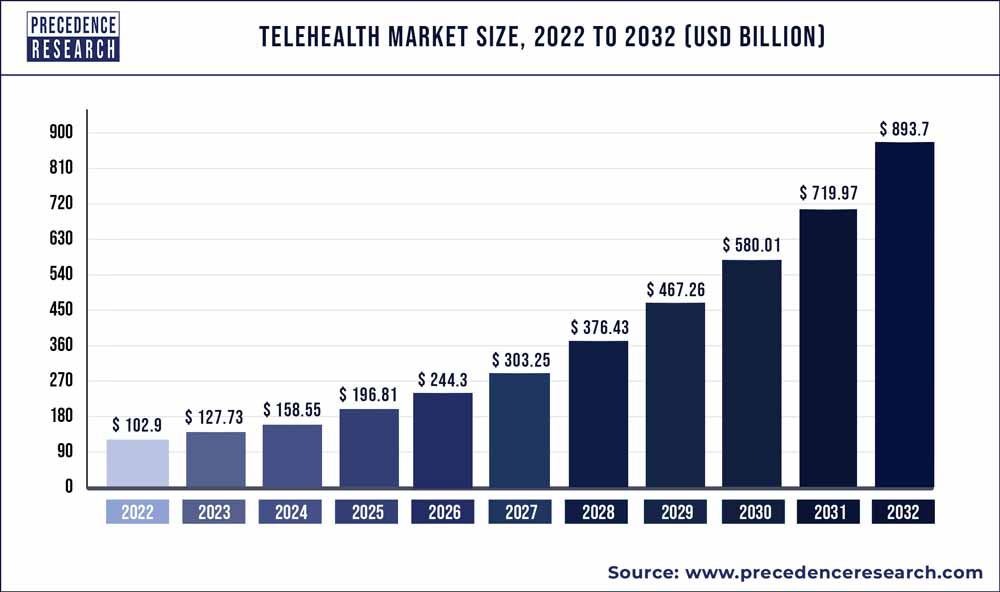
Source: Precedenceresearch
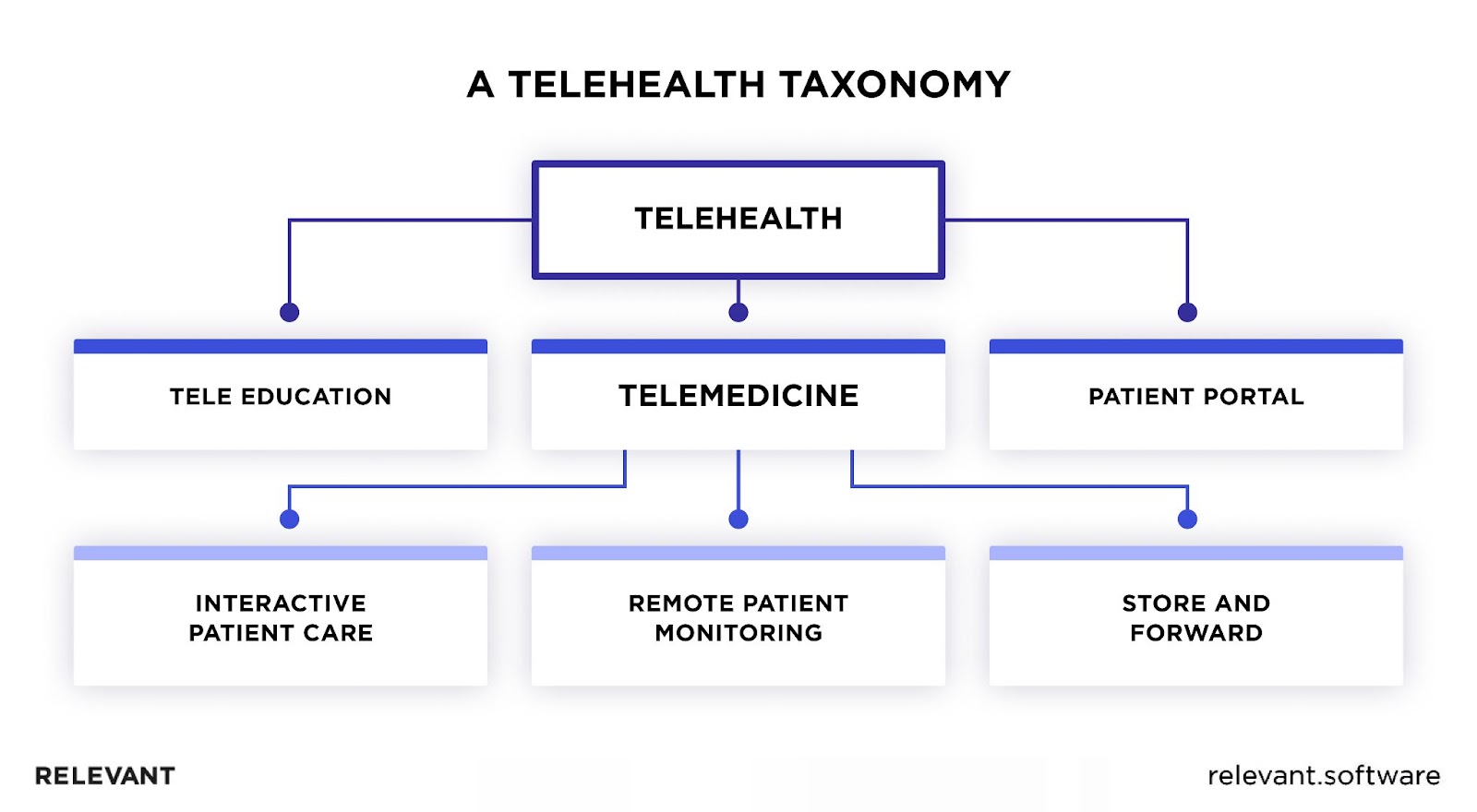
Components of Telehealth
Telehealth, often perceived as merely a digitization of healthcare practices, is far more complicated and multifaceted due to various tools and strategies. Each plays a crucial role in this modernized healthcare model.
- Remote Patient Monitoring (RPM): Patients use specific equipment or wearable tech to send crucial health metrics – heart rhythm, sugar levels, or blood pressure – to medical experts. This process allows for proactive care, paving the way for timely medical intervention. For a full insight into the benefits of remote patient monitoring, take a look at this article.
- Store and Forward (SaF): Different from live interaction, this method involves gathering, storing, and then sending patient data – from diagnostic scans to critical medical details – to specialists for later evaluation and feedback.
- Mobile Health (mHealth): As mobile phones become omnipresent, health-focused apps allow patients to track health stats, book doctor visits, or get initial medical advice. In doing so, they transform our everyday devices into essential health monitoring apparatus.
- Video Consultations: These aren’t just simple virtual chats. These sessions aim for a thorough patient evaluation, medical advice, and, sometimes, specific therapeutic discussions. They aspire to mimic the depth of face-to-face meetings without the associated hassles.
- Interactive Patient Portals: These digital hubs offer patients access to their medical records, the ability to schedule or change visits, and manage prescriptions, giving patients more control over their health journey.
At its heart, Telehealth is an integrated approach where every tool contributes to reshaping modern healthcare.

Applications of Telehealth
Telehealth’s applications span far more diverse areas than one might initially think. Let’s explore how Telehealth impacts different healthcare scenarios:
- Chronic Disease Management: For individuals dealing with ongoing conditions like diabetes, regular medical visits can be exhausting. Telehealth platforms offer a way to keep track of one’s health metrics and communicate with providers, all without those frequent hospital visits.
- Mental Health Sessions: The importance of mental health has been gaining deserved attention lately. Through telehealth, patients can access therapists or counselors from the comfort of their homes.
- Post-operative Care: After surgery, patients need close monitoring. But does it always require staying in the hospital? With telehealth, many post-op check-ins and consultations can be done remotely.
- Pediatric Consultations: For a worried parent, every sneeze of their child can sound like an alarm bell. Telehealth offers quick consultations, letting pediatricians advise whether it’s just a cold or something needing more attention.
- Dermatology: Instead of waiting weeks for an appointment, patients can send images of their skin concerns to dermatologists. Quick, easy, and efficient.
- Rural Health: For those living far from major medical hubs, telehealth is nothing short of revolutionary. It delivers top-tier expertise right to your doorstep, overcoming distance challenges
In essence, the strong side of telehealth lies in its versatility. It’s not just a tool; it’s a toolbox equipped with various solutions tailored for diverse healthcare needs.
Pros and Cons of Telehealth
In an era where digital integration rapidly transforms multiple sectors, healthcare is a prominent beneficiary. As a manifestation of this integration, telehealth presents a palette of advantages while also inviting certain reservations. Let’s weigh the telehealth pros and cons.
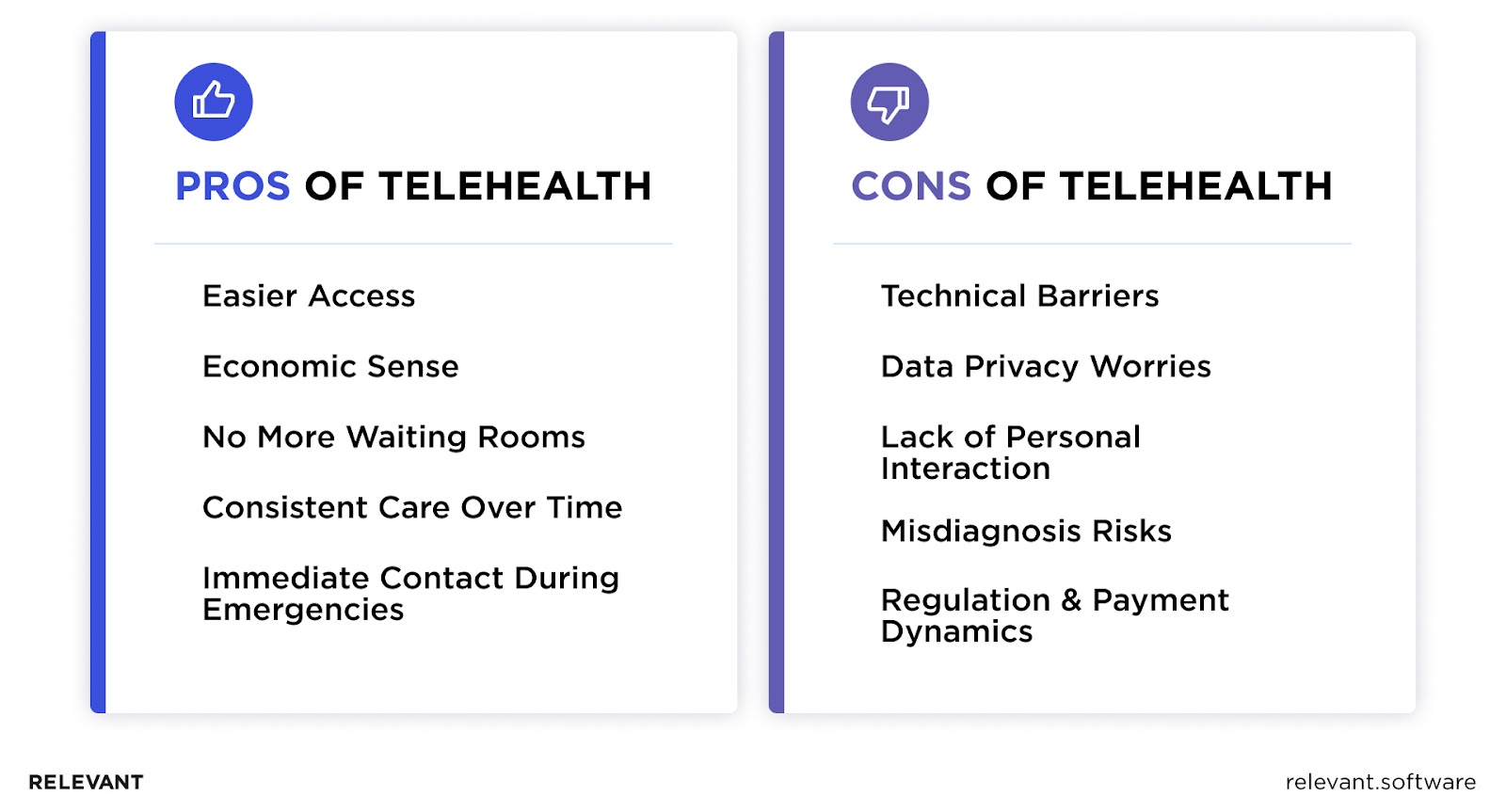
Advantages of Telehealth:
- Easier Access: Telehealth isn’t just about convenience; it’s a lifeline for those in distant places or for individuals with physical limitations. It’s about ensuring that everyone, no matter where they are, has a fair shot at quality healthcare.
- Economic Sense: Not every health concern requires a physical trip to the doctor. Sometimes, a consultation via video can address the issue, and, in the process, save money for both the healthcare provider and the patient.
- No More Waiting Rooms: Many of us know the tiresome of sitting in a waiting room, glancing at the clock every few minutes. Telehealth eliminates that wait, allowing patients to engage with doctors without leaving their living rooms.
- Consistent Care Over Time: With the convenience of virtual check-ins, patients find it simpler to maintain regular interactions with healthcare professionals. This consistency invariably enhances long-term health management.
- Immediate Contact During Emergencies: When rapid medical evaluation is imperative, telehealth platforms emerge as the preliminary assessment point, steering decisions regarding the necessity of physical medical intervention.
Disadvantages of Telehealth:
- Technical Barriers: The prerequisite of robust Internet connectivity and specific digital devices can inadvertently alienate a segment of the population, restricting Telehealth’s universal appeal.
- Data Privacy Worries: The digital realm is not devoid of threats. There are genuine concerns about the integrity of patient data and the looming menace of potential security violations.
- Lack of Personal Interaction: Despite technology’s giant strides, a segment of both healthcare providers and patients believe that virtual interactions can’t replicate the warmth and personal rapport that comes with face-to-face consultations.
- Misdiagnosis Risks: Without a hands-on physical examination, there is a chance that all symptoms or health indicators will be not detected, potentially leading to diagnostic errors.
- Regulation & Payment Dynamics: Telehealth often faces established regulatory parameters, and in many regions, the financial compensation models are yet to evolve to fully encompass its varied offerings.
While Telehealth marks a new dawn in healthcare accessibility and convenience, it’s crucial to approach it with a balanced perspective, recognizing its transformative potential and the challenges it presents.
What is Telemedicine?
Telemedicine signifies the fusion of healthcare and technology, offering clinical services remotely. Though it seems innately contemporary, its seeds were sown in the early 20th century when radiographic images journeyed through telephone lines.
Telemedicine has transformed with technology’s present-day evolution and the ubiquity of the Internet. It’s no longer merely about distant consultations. Today, it spans regular health assessments to intricate, robot-assisted procedures supported by instantaneous data sharing. Its essence? Telemedicine democratizes healthcare. It promises that geographical barriers or limited resources shouldn’t deter one from obtaining timely, expert medical care.
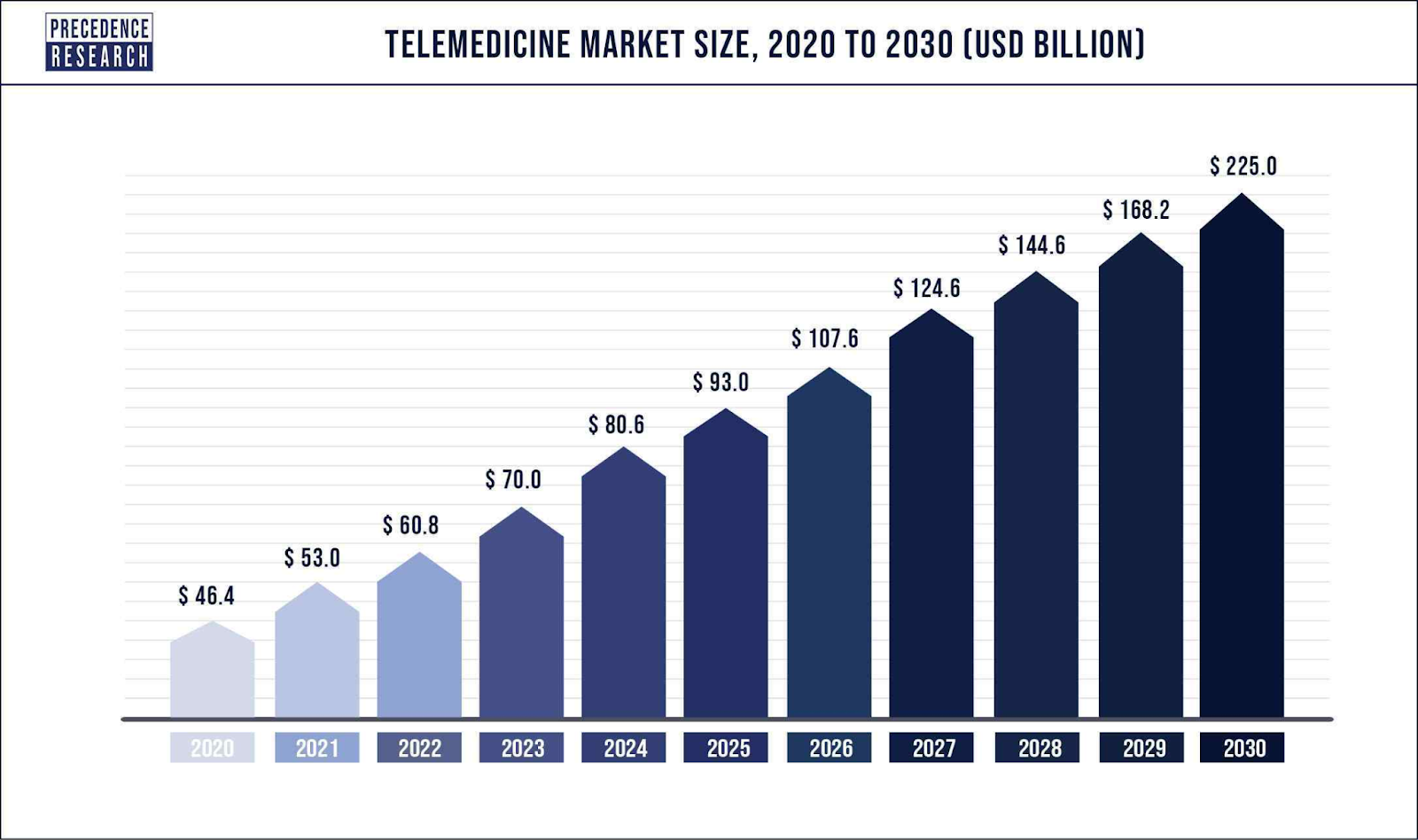
Source: Precedenceresearch
Components of Telemedicine
Telemedicine, a subset of telehealth, concentrates purely on the clinical application of remote healthcare. Unlike telehealth’s broader range, telemedicine’s components are firmly rooted in direct patient care:
1. Clinical Services: This segment focuses on activities like virtual doctor-patient consultations, subsequent follow-ups, drug regimen evaluations, or even discussions with specialists. It all hinges on contemporary tech, predominantly video chats, to simulate that face-to-face doctor’s visit experience.
2. Diagnostic Telemedicine: Ever had an X-ray or an EKG and wondered about the immediate interpretations? This domain specializes in the distant review of diagnostic reports and images. The field of Radiology offers a prime example. Radiologists, even when far away, can swiftly interpret scans, ensuring patients don’t hang in the balance.
3. Telemedical Gear: It’s all about those tailored gadgets crafted for telemedicine. We’re talking about items like the high-tech stethoscope or the otoscope that beams clear images to the other side of the screen. During those online consultations, such tools become indispensable, offering clinicians a clearer perspective.
4. Electronic Health Record Connectivity: Now, this is where tech flexes its muscles. It ensures your telemedicine tool speaks the same language as your doctor’s record-keeping system. So, when your consultation wraps up, everything from the doctor’s notes to specific observations automatically finds its way to your health file.
5. Prescription Workflow: Here’s a neat feature of many telemedicine platforms – the ability for the doctor to directly send prescriptions to your preferred pharmacy, ensuring your treatment doesn’t skip a beat.
In essence, telemedicine redefines and reshapes traditional healthcare, offering a balanced mix of tech prowess and medical expertise in healthcare app development.

Applications of Telemedicine
Over the years, telemedicine has expanded its reach, proving indispensable in various healthcare scenarios. Here’s a closer look at how it’s making a difference:
- Chronic Disease Oversight: Think about those dealing with conditions such as diabetes or heart disorders; their well-being hinges on consistent medical oversight. Telemedicine steps up by erasing distances, letting physicians consistently monitor a patient’s health, make necessary treatment tweaks, and provide guidance, sidestepping the need for repetitive in-person appointments.
- Specialist Engagements: Imagine living in a small town, hours away from specialized medical expertise. This is precisely the scenario where telemedicine stands out. It grants patients an opportunity to touch base with seasoned experts from different corners of the world, ensuring they aren’t deprived of quality medical counsel, no matter where they reside.
- Remote psychotherapy: The importance of consistent therapy and counseling sessions in mental health can’t be emphasized enough. With the challenges that sometimes come with in-person meetings, telemedicine offers a reliable alternative. It ensures individuals can maintain their regular therapeutic interactions, creating a stable healing process.
- Follow-ups Post Treatment: Once a surgical procedure or treatment wraps up, the journey isn’t always over. Patients often need subsequent checks. Telemedicine removes the hassle of travel for these short but vital consultations. It offers a virtual space for practitioners to gauge recovery progression, tackle arising issues, and fine-tune care plans.
- Overseeing ICU Patients: Consider the need for constant vigilance for ICU patients. Telemedicine ensures that, even when a specific specialist isn’t available physically, they can still keep an eye on critical patients, process live data feeds, and work alongside the on-premises medical crew to guide care.
Pros and cons of telemedicine
Telemedicine is reshaping how we think about healthcare. It’s got a lot going for it, but like everything else, it’s not perfect. Let’s break down telemedicine’s pros and cons.
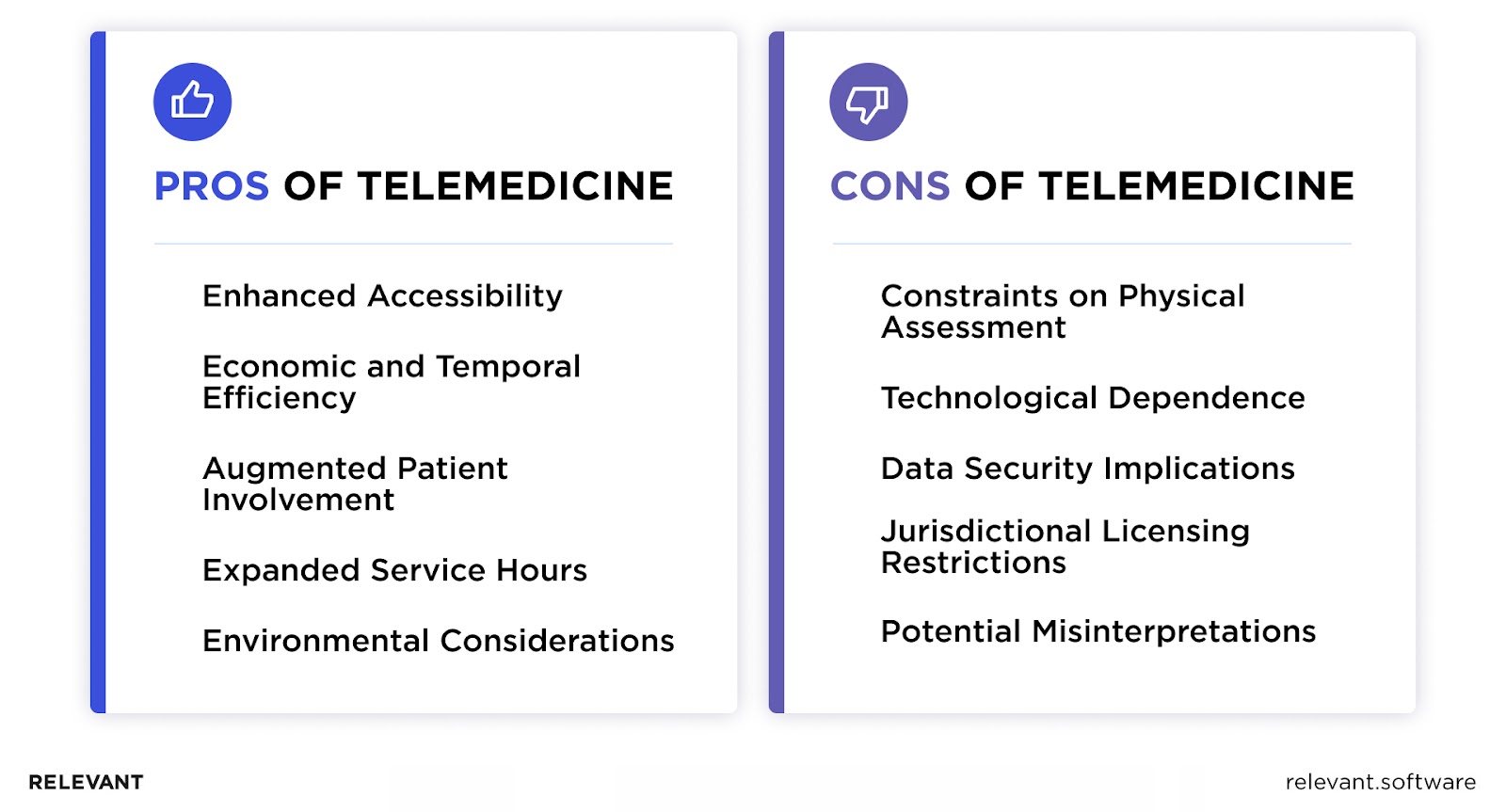
Advantages of Telemedicine:
- Enhanced Accessibility: Telemedicine is especially beneficial for individuals in rural areas or places with a shortage of medical specialists, allowing them to receive expert consultations without the constraints of geography.
- Economic and Temporal Efficiency: Patients’ traditional clinic waiting times are curtailed, while physicians experience improved appointment management.
- Augmented Patient Involvement: Being able to avail medical services from one’s residence often leads to improved patient involvement and greater commitment to prescribed treatments.
- Expanded Service Hours: Medical practitioners now have the ability to extend their services beyond traditional working hours. This facilitates appointments during hours that may be more accommodating for some patients, such as the evening.
- Environmental Considerations: The reduced necessity for patients to travel for consultations directly translates into fewer vehicle emissions, advancing a greener healthcare model.
Limitations of Telemedicine:
- Constraints on Physical Assessment: Not all medical conditions are conducive to remote evaluations. There are situations where an in-person clinical assessment is paramount to ensuring accurate diagnoses. In such cases, telemedicine may not be the most suitable approach.
- Technological Dependence: The effectiveness of a telemedicine consultation hinges on the reliability of the technology used. Issues ranging from connectivity interruptions to hardware failures can compromise the consultation experience for both patients and healthcare providers.
- Data Security Implications: Digital platforms, while efficient, expose sensitive patient information to potential security breaches. Even with robust data protection measures in place, the inherent vulnerabilities of online communications cannot be wholly eliminated.
- Jurisdictional Licensing Restrictions: The often regional nature of medical licensing introduces complications. For practitioners wishing to consult with patients outside their licensed jurisdiction, there can be bureaucratic and legal challenges.
- Potential Misinterpretations: The lack of physical presence in telemedicine consultations might lead to potential communication discrepancies. Without the benefit of face-to-face interaction, nuances might be missed, and instructions or feedback could be misinterpreted.
In summation, while telemedicine presents numerous benefits and innovations in healthcare delivery, it also introduces its set of distinct challenges. True efficacy in this domain will be achieved by amplifying its strengths and diligently addressing its limitations.
Your next read: How does telemedicine work
Telehealth vs Telemedicine: A Comparative Analysis
So what is the difference between telehealth and telemedicine? Here’s an expert breakdown comparing these two concepts across various dimensions.
| Criteria | Telehealth | Telemedicine |
| Scope and Applications | Encompasses a broad spectrum of remote healthcare services, including non-clinical services such as training, administrative meetings, and education. | Primarily leverages video conferencing tools designed for clinical interactions alongside specific diagnostic tools that can be used remotely. |
| Technology and Infrastructure Requirements | Requires a more diverse set of technologies given its broader scope. This may include video conferencing tools, mobile health apps, remote patient monitoring systems, and electronic data storage. | Regulatory aspects predominantly center around patient care, confidentiality, and data protection. Licensing often poses a challenge, given the cross-border nature of services. |
| Accessibility and User Experience | Telehealth services can be accessed across various platforms and may cater to both healthcare professionals and patients. The range in services means the user experience can vary widely. | Telemedicine platforms are specifically designed for patient-provider interactions, usually ensuring a streamlined and patient-friendly experience. |
| Legal and Regulatory Aspects | Given its wide range of services, the regulatory landscape is complex. Policies may differ depending on the specific service being provided. | Regulatory aspects predominantly center around patient care, confidentiality, and data protection. Licensing often poses a challenge given the cross-border nature of services. |
| Cost and Efficiency | Costs can vary based on the technology, service, and infrastructure required. Efficiency gains are witnessed in areas like training and education, reducing the need for physical presence. | Telemedicine can lead to significant savings by reducing the need for in-clinic visits, thereby lowering operational costs and potentially healthcare costs for patients. |
This table provides a snapshot of the variances of telemedicine vs. telehealth. While both are revolutionizing the way healthcare is delivered and consumed, understanding their nuances aids healthcare professionals, policymakers, and patients in optimizing their use.
Telehealth vs Telemedicine: Bottom Line
In the nuanced field of digital healthcare, differences between telemedicine and telehealth might seem subtle but are significant. But why get bogged down by these details when you have a partner like Relevant?
With our decade-long knowledge of healthcare web development and astute IT consulting services, you’re poised to redefine patient care standards. Aspiring to leverage digital advancements? Our healthcare software solutions are meticulously designed for the sector’s distinct demands. Choosing Relevant Software is essentially choosing to be at the cutting edge of healthcare innovation.
FAQ
What are the main pros and cons of telemedicine?
Telemedicine makes healthcare more accessible and often cuts costs. On the flip side, for conditions that need a hands-on check, it might not be the best fit. Plus, technology isn’t foolproof; glitches can happen.What are the main pros and cons of telehealth?
Telehealth covers more ground, from patient education to remote monitoring. It keeps patients engaged and informed. But, as with anything online, there’s always that niggling worry about data security. Also, some folks miss the warmth of in-person chats.What are the important differences between telemedicine and telehealth?
It’s a common mix-up! Think of telemedicine as a subset. It’s all about remote clinical services. Telehealth is the umbrella term, covering not just clinical services but also things like health education.What hardware and software are used for telemedicine?
Doctors use a mix of gadgets and software. They might use digital stethoscopes or specific cameras to get a closer look. Software-wise, they’ll use video chat tools and systems to manage patient info securely.How does telemedicine reduce costs?
Fewer brick-and-mortar clinics mean less overhead. Plus, patients are less likely to skip appointments, which means more consistent revenue. And with remote monitoring, fewer unnecessary hospital visits can save tons of money.How does telehealth improve patient care?
It’s all about breaking down barriers. Patients can get care or advice promptly, even if they’re miles away from a clinic. For those with long-term conditions, it means more regular check-ins, which can be a game-changer.

Hand-selected developers to fit your needs at scale! Let’s build a first-class custom product together.

