Behind the Screen: How Does Telemedicine Work in Today's World?

In an era where we order meals with a touch, explore far-off places without leaving our living rooms, and instantly keep in touch with family on the other side of the world, shouldn’t our health experiences be just as painless? That’s where telemedicine steps in—a harmonious fusion of cutting-edge tech and healthcare, envisioning a reality where nurturing care meets the handiness of the digital era.
Remember those days when a doctor’s visit meant navigating city traffic, enduring seemingly endless waits, and occasionally braving a space filled with sneezes and coughs? Telemedicine is rewriting that narrative, offering a modern, patient-friendly approach to healthcare. It’s more than just seeing your doctor on a screen; it’s a holistic framework crafted to bring healthcare closer, make it swiffer, and, surprisingly, more intimate.
from 25 countries outsourced software development to Relevant
We provide companies with senior tech talent and product development expertise to build world-class software.
Yet, as we find ourselves at this promising crossroads, we must clarify: “How does telemedicine work?” How does it change the way we perceive healthcare, transform doctor-patient engagements and care practice? Dive into this piece, where we explain this groundbreaking shift.
What is Telemedicine?
Envision a reality where distance and time aren’t obstacles to getting quality medical care. This is the promise telemedicine seeks to fulfill. Fundamentally, telemedicine seeks to erase the geographical and temporal gaps that once separated patients from healthcare providers. Rather than facing long commutes or tiring waits, accessing medical insights is now as straightforward as dialing a number.
But to view telemedicine merely as a virtual doctor’s appointment sells it short. It’s a complex, adaptive system that offers myriad solutions, each sculpted to meet the diverse needs and situations that healthcare presents.

Types of Telemedicine
Diving deeper into the world of telemedicine, it’s essential to understand that it’s not a monolithic entity. Just as there are diverse medical needs, telemedicine too has various types, each designed for specific situations and services. Let’s explore these and get a clearer picture of the breadth and depth of telemedicine.
- Store-and-Forward (Asynchronous Telemedicine): It’s like sending a postcard to a specialist, but digitally. A primary care physician, for example, might send over a snapshot of a rash, and a dermatologist could then review and share insights—all without needing to sync up in real time.
- Real-Time (Synchronous Telemedicine): This is the face of telemedicine that most people recognize. It’s direct, real-time interaction, similar to a video call. Whether you’re having a routine chat, discussing your mental well-being, or revisiting a previous ailment, this format offers instant connectivity and advice.
- Remote Patient Monitoring (RPM): Think of it as having a vigilant, silent medical assistant. Patients employ IoMT devices that keep a watchful eye on their health metrics, such as blood pressure or sugar levels. These readings are then transmitted for medical professionals to monitor, offering proactive and timely care, especially crucial for chronic illnesses. Discover more about the benefits of Remote Patient Monitoring here.
- Mobile Health (mHealth): Our smartphones are glued to our hands, so why not employ them for better health? mHealth rides the wave in healthcare app development to optimize our wellness journeys. Be it reminders for your meds or monitoring your mental well-being, this form of telemedicine slots health into our pockets.
At its heart, telemedicine is a dynamic addition to the healthcare realm, adapting to the rhythm of our digital age, making patient care more immediate, individualized, and in tune with our times.

How Does Telemedicine Work: The Process
From the various telemedicine examples, we see today to the cutting-edge telemedicine software solutions powering these platforms, the world of virtual healthcare is vast. To truly understand it, we need to break down its workflow and see how it operates at each stage.
Patient Registration and Scheduling an Appointment
Before any consultation, the journey starts with the patient registering on telemedicine software platforms. These platforms, lauded as some of the best telemedicine software solutions, have intuitive interfaces making registration a breeze. With a few clicks, patients can schedule their appointment, choosing a time that fits their convenience.
Remote Consultations and Examinations
The heart of telemedicine and ehealth lies in remote consultations. Once registered, patients can seamlessly connect with healthcare professionals. The telemedicine solution ensures that the consultation experience is almost akin to being in a doctor’s office. Tools are embedded to allow doctors to perform remote examinations, making virtual check-ups as comprehensive as in-person visits.
Diagnosis and Treatment Plans
Post-consultation, doctors employ the telemedicine workflow to make a diagnosis and formulate treatment plans. They have access to integrated medical databases, ensuring their diagnosis is informed by the latest in medical research. In addition, you can easily connect professionals, contributing to joint assistance.
Electronic Prescriptions and Follow-up
One significant advantage of telemedicine is the ability to generate and send electronic prescriptions directly to the patient or their chosen pharmacy. Patients no longer have to worry about misplacing their prescription receipts. Plus, scheduling follow-ups is effortless, allowing patients to discuss progress, concerns, or changes in their condition.
Billing and Insurance in Telemedicine
Last but not least is the monetary aspect. Integrating billing and insurance into the telemedicine solution simplifies the process for both the provider and the patient. In-built tools help handle insurance claims, and e-billing ensures patients can settle their dues without the hassle of paper bills.
In specialized areas like telemedicine pain management, the entire process becomes even more crucial, as consistent communication, timely interventions, and effective follow-ups can drastically improve patient outcomes.
Telemedicine vs. Telehealth: Do They Differ?
In the era of digital health revolutions, two terms often surface in discussions, webinars, and even at renowned telemedicine conferences: telemedicine and telehealth. While they might sound synonymous, and many use them interchangeably, there are nuances that distinguish one from the other. It’s akin to comparing the software behind a video call to the entire ecosystem of digital communication. Let’s delve deeper into these terms and shed some light on their distinctions.
Telemedicine primarily focuses on the clinical aspects of remote healthcare. When you think of a doctor providing a consultation via video call, you’re thinking of telemedicine. The telemedicine video conferencing software, an essential part of this domain, ensures that patients and doctors can interact with clarity, precision, and real-time feedback, making these virtual consultations as effective as in-person visits.
Telehealth, on the other hand, casts a broader net. It encompasses the entirety of remote healthcare services and education. This includes non-clinical services such as training, administrative meetings, and continued medical education, often facilitated through diverse platforms. So when you attend telemedicine conferences, witnessing discussions ranging from policy changes to software demos, you’re witnessing telehealth in action.
Implementation-wise, introducing telemedicine typically means incorporating tools and protocols that facilitate virtual doctor-patient interactions. Telemedicine implementation might involve selecting the right video conferencing software, ensuring secure data storage, and training healthcare providers in its effective use. Telehealth implementation, meanwhile, is a broader endeavor, spanning everything from patient education initiatives to remote health monitoring tools.
To draw an analogy: If telemedicine were a gripping novel, telehealth would be the entire library. One is a chapter, albeit an essential one, while the other represents the complete story.
So the next time you find yourself navigating the world of virtual healthcare, equipped with an understanding of the difference between telemedicine and telehealth, you’ll appreciate the depth and breadth of innovations that are redefining the future of healthcare.

The Bright Side: Exploring Benefits of Telemedicine
In the setting of healthcare evolution, telemedicine stands out as an invisible line, weaving new possibilities and knitting the world a bit closer. The concept is simple: melding the power of telecommunications in healthcare with the foundational principles of medical service. Let’s explore the profound benefits this merger brings to the fore.
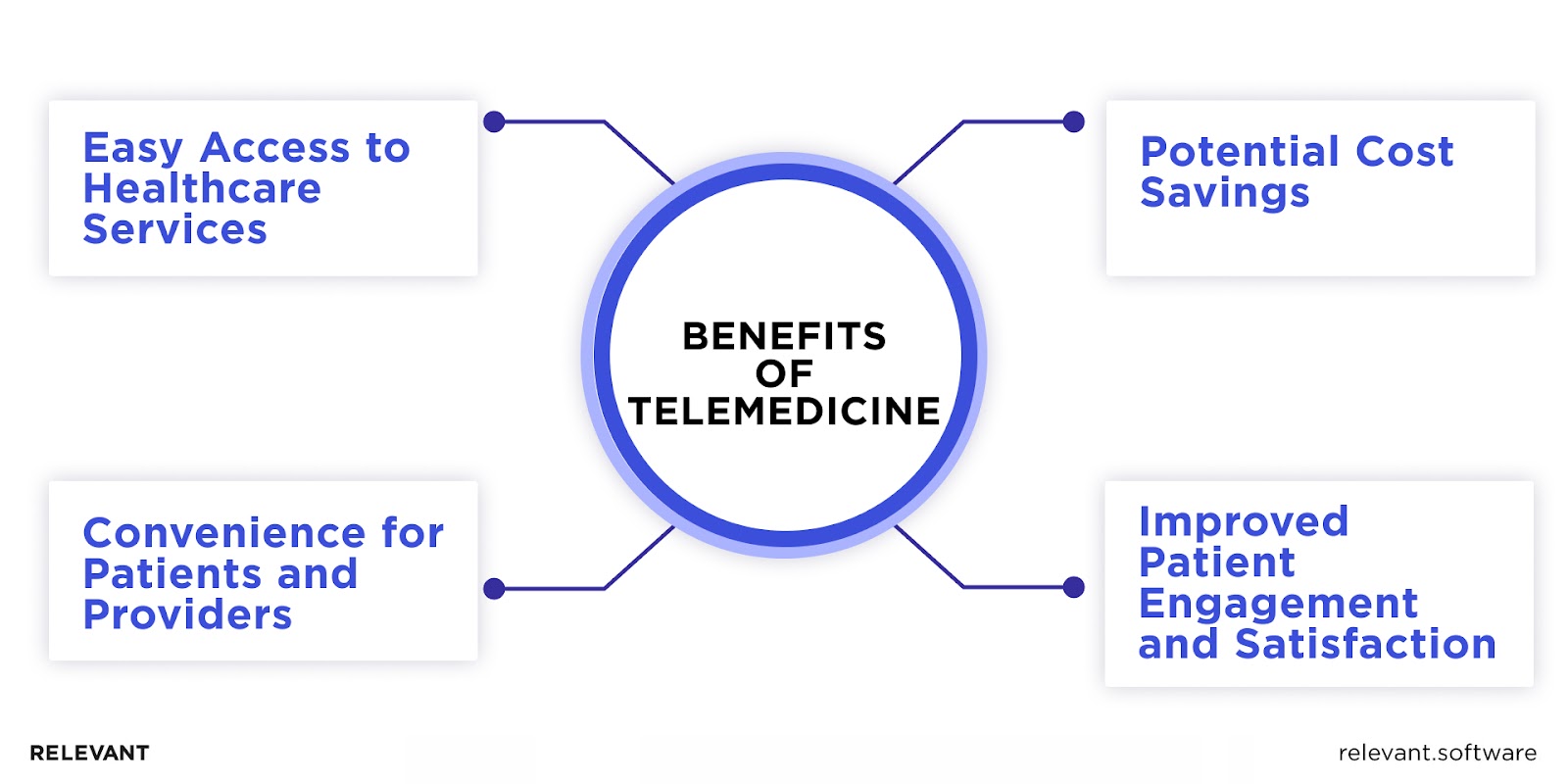
Easy Access to Healthcare Services
Gone are the days when geographical boundaries dictated healthcare accessibility. With video conferencing in healthcare, a patient in a remote village can virtually step into a doctor’s cabinet in a bustling city. International telemedicine laws are increasingly embracing this, fostering a global healthcare community that transcends borders. This democratization ensures that regardless of where you reside, quality healthcare isn’t out of reach.
Convenience for Patients and Providers
Imagine swapping the hours spent in traffic and the waiting room for the comfort of your living room. That’s telemedicine for the patient. Now, envision a doctor’s ability to schedule a consultation appointment around surgeries, research, and even personal commitments. That’s telemedicine for the provider. It’s more than just connecting healthcare; it’s about streamlining it to cater to modern-day patient needs and professional demands.
Potential Cost Savings
With brick-and-mortar establishments come overhead costs, which often trickle down to the patient. Telemedicine, by shifting the paradigm to virtual platforms, can alleviate some of these expenses. Reduced transportation costs for patients, lesser infrastructural demands for providers, and the possibility of treating more patients in a day all add up to significant savings potential.
Improved Patient Engagement and Satisfaction
A prominent outcome of telemedicine is the surge in telemedicine patient satisfaction. Maybe it’s the choice of environment for a consultation or the novelty of leveraging technology. When patients feel involved, heard, and valued, their engagement with their health journey naturally amplifies. The ease of follow-ups, promptness of services, and sheer convenience ensure that patients aren’t just recipients of care but active participants.
Telemedicine doesn’t promise to replace traditional medicine. Instead, it offers a complementary path, one that understands the rhythm of our digital age and strives to harmonize healthcare with it. The benefits are clear, and as the world grows more interconnected, the potential of telemedicine is just beginning to unfold.
Drawbacks of Telemedicine
While telemedicine has undoubtedly introduced a paradigm shift in healthcare, offering innovative solutions and convenience, it is not without its challenges. Like any evolving domain, there are teething issues and inherent limitations that need to be addressed to maximize its potential. Let’s examine some of these drawbacks to gain a balanced perspective.
Limitations of Virtual Consultations
The face-to-face interaction in a doctor’s chamber isn’t just about the conversation; it’s also about the unspoken cues—the palpable tension in a patient’s posture, the subtle tremor of a hand, the nuances that sometimes go beyond verbal articulation. While virtual consultations bridge geographical gaps, they can sometimes miss out on these critical human nuances that can be pivotal in a diagnosis or therapeutic relationship.
Technical Issues and Infrastructure Requirements
Relying heavily on technology means telemedicine is only as good as its weakest technical link. Patients and providers can sometimes face dropped calls, low-resolution images, or system crashes. Moreover, both parties need interoperability, reliable internet connections, and updated equipment. This can be especially challenging in remote areas or for individuals who might not be tech-savvy, making the digital divide a genuine concern in the realm of telemedicine.
Regulatory and Licensing Challenges
Navigating the maze of international telemedicine laws (including HIPAA guidelines), licensure requirements, and cross-border regulations can be daunting. What’s permissible in one region might be a regulatory violation in another. This complex web can make it challenging for providers to offer their services globally or for patients to access specialists from other regions.
Ensuring Quality of Care and Patient Safety
Standardizing the quality of care in a digital space is not straightforward. While many telemedicine platforms have rigorous guidelines and quality checks, ensuring consistent patient safety can be tricky. How do you guarantee that a remote diagnosis is as accurate as an in-person one? Or that the treatment recommended via a screen is as effective?
While telemedicine is undoubtedly the future’s direction, acknowledging its drawbacks ensures that the evolution is both thoughtful and focused on the primary goal: holistic, effective, and accessible healthcare for all. As the industry grows, it is essential to continuously refine and address these challenges to make telemedicine an unwavering beacon in healthcare’s future landscape.
Who Can Use Telemedicine?
Hasn’t the blend of technology with everyday life brought wonders to our doorstep? Telemedicine, this exciting intersection of tech and healthcare, often prompts the question: “Who’s it really for?” Well, the breadth of its reach might astonish many.
Imagine a dedicated city professional, juggling meetings and deadlines who squeezes in consultation via telemedicine software right from her high-rise office. Contrast this with a farmer in a secluded countryside, for whom the nearest medical center is a journey away. Yet, with a simple gadget and connectivity, he’s discussing symptoms with a specialist in the city.
It’s not just about patients, though. Doctors, irrespective of their specializations—be they skin experts, heart specialists, or even therapists—are incorporating telemedicine tools into their practices. What’s more, these platforms are also turning into virtual classrooms, equipping the next generation of doctors with knowledge and insights.
How Does Telemedicine Work: Final Thoughts
In a world constantly racing with time, seamlessly blending technology with healthcare was a move waiting to happen. With telemedicine platforms in play, we’re not only crossing physical boundaries but also making healthcare a more inclusive realm. It’s not about replacing the age-old, trusted doctor-patient relationship; it’s about giving it a new dimension, a fresh perspective. So, as we acquaint ourselves more with how telemedicine works, we’re not just learning a concept. We’re embracing a future where healthcare is more personalized, reachable, and attuned to our modern lives.
To really tap into what tomorrow holds, you need someone by your side who gets the techy bits just as much as they appreciate the profoundness of healthcare. Thinking about crafting a state-of-the-art telemedicine platform or giving your existing services a boost? Rely on Relevant`s healthcare software development and healthcare IT consulting services. We’re here to turn your aspirations into tangible outcomes. Reach out to Relevant Software, and let’s shape a future of healthcare hand in hand.
FAQ
How does telemedicine diagnose different illnesses?
Telemedicine employs a combination of detailed patient histories, visual examinations via high-quality video calls, and, sometimes, remote monitoring tools to diagnose a range of ailments. For more intricate diagnostics, doctors might still recommend in-person tests.How do telemedicine appointments work?
Much like a physical appointment, you’d book a slot online, but instead of heading to a clinic, you join a video call. The doctor reviews your medical history, discusses symptoms, and advises accordingly—all from the comfort of your space.What are the main types of telemedicine?
Primarily, there are three: Store-and-Forward (transferring medical data), Remote Patient Monitoring (tracking patient data over time), and Real-Time Interactive Services (live discussions between patient and provider).How does telemedicine improve patient experience?
Telemedicine offers convenience—no travel, no waiting rooms. Plus, it provides increased access to specialists, quicker consultations, and, often, more personalized attention, enhancing overall patient satisfaction.What equipment do you need for telemedicine?
Basic requirements include a computer or smartphone, a stable internet connection, and a camera. Some cases might need specific monitoring devices, but generally, the tech barrier is low, making it widely accessible.

Hand-selected developers to fit your needs at scale! Let’s build a first-class custom product together.

