What is HL7? Healthcare Interoperability & HL7 Standards Explained

Today’s healthcare world is built on digital systems, but those systems only work when they can talk to one another. That’s where HL7 comes in. Instead of keeping data trapped in separate systems, HL7 standards let hospitals, labs, and EHR vendors speak the same language, enabling information to flow smoothly to the right place at the right time. Think of it as the bridge that keeps care teams aligned.
So, what is HL7 in healthcare, and why should it matter to you? Without it, medical records would look like mismatched puzzle pieces. Lab results might arrive late, billing data could get lost, and critical details could be misread at the worst possible time. The difference between smooth interoperability and confusion is often HL7.
from 25 countries outsourced software development to Relevant
We provide companies with senior tech talent and product development expertise to build world-class software.
At Relevant, our experts in healthcare software development services see this every day. A clean HL7 interface can mean faster check-ins at a clinic, fewer repeated tests, and better care decisions. Scroll down and you’ll find a deeper look at HL7’s evolution, the role of CDA and FHIR, and what these standards really mean for the future of connected healthcare.
What is HL7 in healthcare?
HL7 standards are a family of specifications created by Health Level Seven International. Their purpose is simple but critical: to define how healthcare systems format and exchange data. Instead of each hospital, lab, or payer inventing its own rules, HL7 provides a shared playbook that ensures information moves accurately, with context, and reliably across care settings. The impact is fewer custom interfaces, cleaner HL7 data, and faster delivery of information that clinicians depend on.
So, what does HL7 stand for? Health Level Seven. The “Seven” refers to the application layer of the OSI model—the level at which software systems communicate directly with one another. In practice, HL7 is both a set of message formats and a collection of clinical rules that guide the representation and transmission of patient data.
The HL7 family of standards includes several key components:
- Primary standards: Core rules that define how systems communicate and stay compliant.
- Foundational standards: The technical framework and protocols every healthcare organization should follow.
- Clinical and administrative domains: Guidelines for managing documentation and combining structured data with message exchanges.
- Medical system profiles: Practical directions for setting up and managing EHR system behavior.
- Implementation guides: Step-by-step manuals that help teams deploy solutions correctly and efficiently.
- References: Detailed definitions and technical specs for developers building healthcare software.
- Education and awareness: Learning materials that help teams stay updated and adopt HL7 smoothly.
The origin and evolution of HL7 standards
HL7 originated in the 1980s to replace the need for countless custom interfaces between healthcare systems. Version 2 became the main standard for exchanging event messages. Version 3 introduced the Reference Information Model (RIM) and XML. The CDA format standardized how clinical documents are shared. Later, FHIR built on the best parts of earlier versions and adopted modern web APIs. Each step moved healthcare closer to safer, faster, and more consistent data exchange.

Core HL7 standards at a glance
With several versions and types, understanding HL7 standards is pivotal to grasping the present and future of healthcare integration. So, for a start, read about the varying kinds of standards and their role in our ever-evolving healthcare landscape.
- HL7 v2.x – The backbone of healthcare messaging for events like admissions, discharges, transfers (ADT), lab orders and results, schedules, and billing. It uses message segments such as MSH, PID, PV1, OBR, and OBX. Optional fields and custom Z-segments let organizations include local data without breaking compatibility.
- HL7 v3 – A model-based standard built on the Reference Information Model (RIM) using XML messages. It provides richer meaning and consistency, but is more complex, so adoption is smaller than v2.
- CDA (Clinical Document Architecture) – XML-based documents that include both readable text and structured coded data. Commonly used for discharge summaries, consultation notes, and imaging reports.
- FHIR (Fast Healthcare Interoperability Resources) – Uses modular “resources” like Patient, Observation, Encounter, and Medication, shared through REST APIs in JSON or XML. It’s well-suited for web portals, mobile apps, and integration with external systems. For delivery support or audit assistance, see our HL7 FHIR services.
The core components of HL7
HL7 works because every message follows clear building blocks. The standard defines how systems pack data, label it, and confirm delivery so nothing gets lost or misread. In this section, we outline the core components that ensure interfaces are predictable and safe.
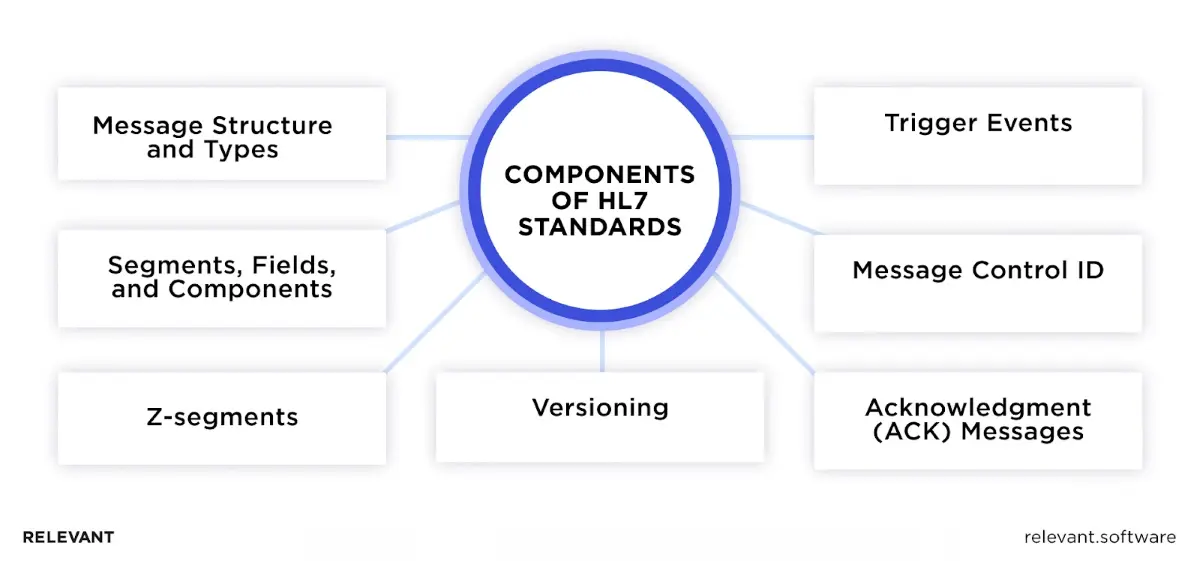
1. Message structure and types
At its core, HL7 organizes messages in a clear, structured hierarchy. Each message type has a specific role, such as registering a patient, sending lab results, or processing billing data. This consistent structure preserves the meaning of each piece of information, enabling receiving systems across healthcare to interpret and use the data accurately.
2. Segments, fields, and components
HL7 messages are divided into segments, similar to sentences in a paragraph. Each segment contains fields (akin to words in a sentence analogy) that convey specific data. These fields can be further broken down into components for even more detail. This meticulous breakdown ensures that each tiny bit of information has its rightful place in the message.
3. Z-segments
Flexibility is key in the dynamic healthcare industry. Z-segments enable users to include custom data segments that may not be part of the standard HL7 definition. This means hospitals and vendors can consist of information specific to their workflows without breaking compatibility, allowing them to adapt messages to their exact needs
4. Trigger events
Trigger events are the actions that initiate HL7 messages. For example, when a patient is admitted, that event triggers the system to send an HL7 message. By standardizing these triggers, HL7 ensures that healthcare systems respond to and share information consistently whenever key events occur.
5. Message control ID
Just as patients need unique IDs, so do their digital records. The Message Control ID assigns a unique identifier to each HL7 message. It ensures that the right message is recognized, processed once, and recorded accurately, even as the system becomes increasingly busy.
6. Acknowledgment (ACK) messages
Communication is a two-way street. When one system sends an HL7 message, the receiving system responds with an ACK message. This response confirms that the message was received and processed successfully or alerts the sender if there was a problem.
7. Versioning
As healthcare and technology advance, the HL7 standard continues to evolve. Versioning helps track these updates and improvements. By clearly stating which HL7 version a system uses, organizations can ensure compatibility and smooth communication, so every system continues to “speak the same language.
The role of HL7 standards in healthcare
What are HL7 standards, and how do they shape daily healthcare operations? Relevant Software experts explain that HL7 serves as the foundation for modern healthcare interoperability, enabling clinical, administrative, and financial systems to exchange data accurately and securely.
- Admissions and patient movement. ADT messages register new patients, update demographics, track bed changes, and discharge patients. They keep EHR, bed management, and billing systems in sync.
- Orders and results. ORM places orders for labs and imaging. ORU delivers results with codes, units, ranges, and timestamps. Clinicians see the correct value in the right chart.
- Scheduling. SIU updates calendars for clinics, operating rooms, and radiology—staff plan resources without double entry.
- Medication workflows. Pharmacy and CPOE systems exchange orders, administrations, and status updates. Safety checks stay intact across systems.
- Clinical documents. CDA transports discharge summaries, consult notes, and imaging narratives. Teams keep a durable, human-readable record with structured data inside.
- APIs and patient access. FHIR exposes resources such as Patient, Encounter, Observation, and Medication via REST. Portals, mobile apps, and partner systems can securely view or update this information.
- Public health and reporting. Interfaces submit immunization records, syndromic surveillance data, and case reports to registries. Agencies act on timely, standardized data.
- Revenue cycle. Demographics, insurance details, and charges pass to billing platforms: fewer denials and faster claims.
- Analytics and AI. Clean HL7 feeds power population health, quality measures, and clinical decision support. Data moves with context and provenance.
That is how HL7 delivers healthcare interoperability in practice: clear events, standard structures, and predictable interfaces that support safer, faster care.
The major benefits of HL7 in healthcare
How is HL7 used in healthcare? These standards have become the backbone of health data exchange, not just as a technical framework but as a driver of safer, faster, and more efficient care. Here are the most essential advantages in practice.
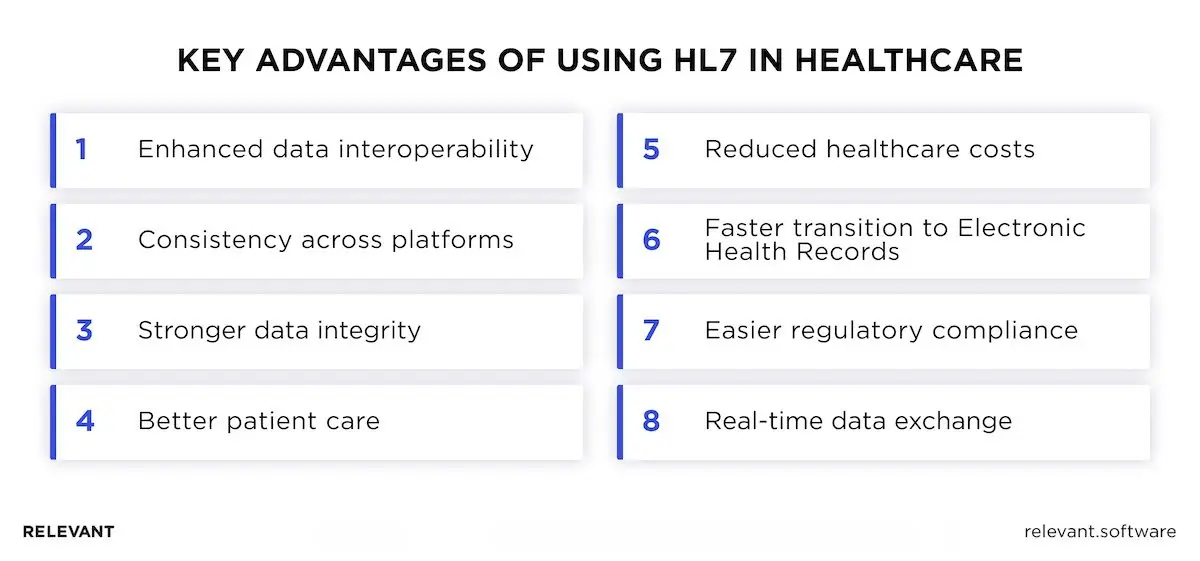
Enhanced data interoperability
The challenge of interoperability — systems failing to share information — has long shaped the healthcare landscape. HL7 solves it by creating a universal format that lets diverse platforms connect, improving efficiency behind the scenes and delivering better care up front.
Consistency across platforms
With HL7, the frustration of interpreting data in different formats disappears. Whether the source is an EHR, a lab system, or a billing tool, the information arrives in a predictable, standardized form that is easy to use.
Stronger data integrity
Every HL7 message adheres to rules that safeguard data during transmission. That structure reduces duplication and prevents corruption, so the results entered by a lab technician reach the treating physician intact.
Better patient care
At the heart of healthcare is —and should always be —the patient. By streamlining how data is shared, HL7 enables medical professionals to obtain a complete view of a patient’s history, helping them make more accurate diagnoses and deliver timely care.
Reduced healthcare costs
Every repeated test or manual data entry adds unnecessary cost. HL7 reduces this waste by improving data sharing and eliminating duplication. That means both savings for providers and better value for patients.
Faster transition to Electronic Health Records (EHRs)
Switching from paper charts to digital records has been one of healthcare’s biggest hurdles. HL7 provides the framework that makes this transition smoother. Instead of reinventing the wheel, organizations can use proven messaging standards to get Electronic Health Records projects moving.
Easier regulatory compliance
Rules around privacy and safety are complex. HL7 provides a framework that aligns with these regulations, helping hospitals and clinics stay compliant without having to build everything from scratch. It’s a compass through a regulatory maze.
Real-time data exchange
In critical scenarios, delays can cost lives. HL7 enables near-instant data exchange so updates on admissions, lab results, or medications reach the right people at the right time.
Challenges and solutions in HL7 implementation
HL7 implementation feels like organizing a dynamic boardroom meeting where the agenda keeps shifting. It’s a challenge, no doubt, but it’s one that we’re tackling with both strategy and agility. So, let’s break down the specifics and see how we’re streamlining the process.
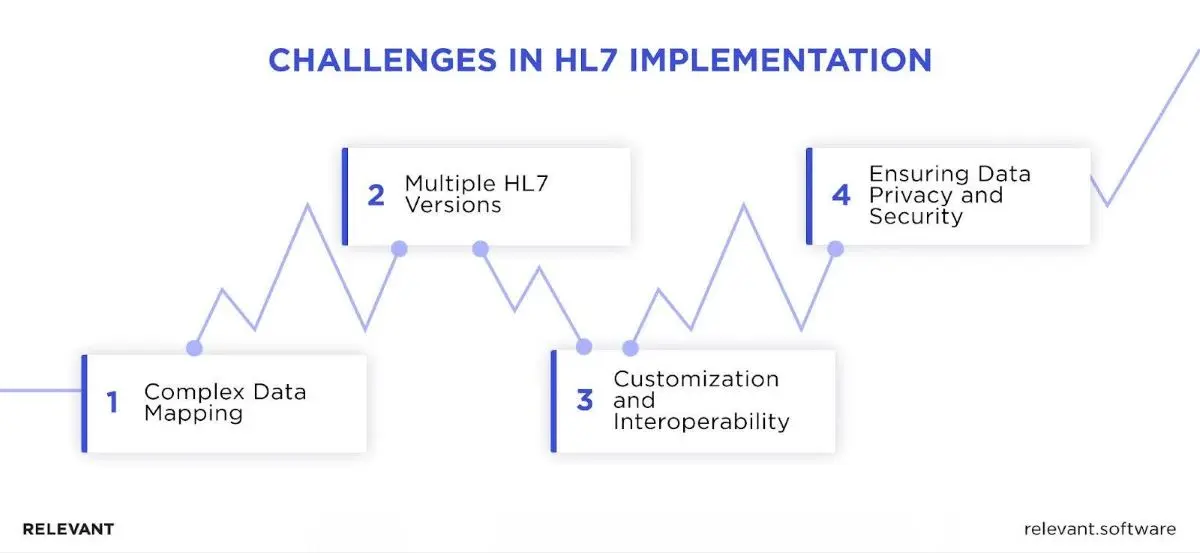
Complex data mapping
The challenge: Every healthcare system has its own way of structuring information. When one EHR records “blood pressure” differently from another, confusion can arise, and data may lose meaning
The solution: You can’t solve this problem with a glossary alone. The honest answer lies in building a strong translation framework. With advanced interface engines handling the heavy lifting and IT teams trained to spot issues early, we make sure complex data doesn’t get lost in the shuffle. It’s a careful process, but one we’ve learned to manage with accuracy.
Multiple HL7 versions
The challenge: Unlike a static framework, HL7 is constantly evolving. New releases refine the standard, but uneven adoption leaves systems out of sync. Imagine trying to finalize a deal where each participant is quoting a different draft. That’s the challenge of multiple HL7 versions.
The solution: Standardize where possible and document every interface. Gateways and integration engines can translate between versions without forcing changes in core systems. By synchronizing upgrades and locking down profiles, organizations maintain consistent communication even as HL7 evolves.
Customization and interoperability
The challenge: No two healthcare organizations are exactly alike. Custom Z-segments and optional fields solve local needs but can undermine interoperability if left unchecked.
The solution: HL7 provides a reliable structure that promotes common understanding across systems, while also supporting limited customization. This means healthcare organizations can address their own requirements without stepping outside the shared interoperability language.
Ensuring data privacy and security
The challenge: Healthcare organizations treat data as both a vital resource and a vulnerable asset. Sharing it improves care, but exposure creates risk. The challenge is to enable continuous exchange while shielding every detail from unauthorized access.
The solution: Safeguarding health information means more than moving data around. HL7 protects through modern encryption, ongoing oversight, and strict access controls. These measures turn the standard into a reliable shield, ensuring records remain private while still available to clinicians who need them.
Current trends influencing HL7 standards
The push for healthcare interoperability continues to accelerate. Hospitals, payers, and vendors now expect systems to connect with less friction and more traceability. HL7 — the broader Health Level Seven standards — remain the base. The change is how teams deliver them in real programs across EMR platforms, partner apps, and analytics stacks.
The shift toward FHIR
FHIR has become the most influential standard, changing the way organizations approach healthcare interoperability. Instead of large, complex payloads, it uses modular “resources” for Patient, Encounter, Observation, and clinical documents like discharge summaries.
This design makes FHIR in healthcare easier to test, secure, and scale. A strong FHIR implementation requires clear profiles and conformance testing to ensure that every EMR and partner system interprets data consistently. Many hospitals now run a hybrid model: v2 for admissions, CDA for long-form records, and FHIR APIs for apps, portals, and external connections.
SMART on FHIR
One of the most significant advances in health level seven standards is SMART on FHIR. This framework uses OAuth 2.0 to authorize apps safely and predictably, with explicit permissions for each purpose. For example, a doctor can open an app within the EMR that accesses only the data needed for a specific task, while patients can do the same from their portals—audit logs track who accessed what and when. By standardizing how FHIR apps connect, SMART increases security, builds trust, and speeds up the delivery of new healthcare tools, making large-scale interoperability safer and faster.
Impact of cloud computing
Cloud computing is no longer a side option in healthcare; it’s the backbone of many integration projects. Instead of running everything on local servers, organizations can now scale HL7 data standards workloads—from high-volume v2 traffic to modern FHIR APIs—through managed cloud platforms.
This shift means less time tied up in hardware maintenance and more focus on delivering clinical value. Security still comes first: encryption, access controls, and compliance with HIPAA or GDPR remain non-negotiable. When done correctly, the cloud strengthens disaster recovery, streamlines analytics pipelines, and makes patient data both easier to access and more dependable across the healthcare system.
APIs for healthcare data exchange
APIs now sit at the heart of healthcare interoperability. As HL7 shifts toward web-ready design, RESTful APIs provide systems with a cleaner way to communicate without the need for custom parsers. FHIR defines resources, search parameters, and error handling, while SMART on FHIR ensures secure app connections.
Together they power entire ecosystems, from Apple Health Records to Epic’s App Orchard. APIs also let clinical documents travel alongside structured data, so narrative context and coded values move together. For developers, this means faster delivery and fewer surprises. For patients and clinicians, it means timely access to trustworthy information.
FHIR vs HL7
Think of these standards as the established brand of healthcare data exchange. For decades, HL7 v2 and CDA have given hospitals, labs, and payers a reliable way to share information. They are proven, widely deployed, and still form the backbone of most HL7 hospital integration projects today.
Now picture FHIR as the newest product line from that same brand — modern, modular, and built with today’s developers in mind. FHIR brings together HL7’s clinical precision with modern web technologies like XML, JSON, and REST. Instead of bulky messages, it organizes information into small, reusable “resources” that connect like LEGO blocks. This design makes FHIR easier to adopt, test, and extend, especially for mobile apps, patient portals, and third-party solutions.
The momentum behind FHIR is strong. Governments are actively pushing it: Germany has required FHIR interfaces in its national programs, while the U.S. 21st Century Cures Act mandates FHIR-based APIs for patient access. These policies underscore FHIR’s role as the next step in healthcare interoperability, without replacing the foundation that HL7 v2 and CDA continue to provide.
Read also: FHIR vs HL7.
Partner with Relevant Software for HL7 integration
Modern standards, new technologies, and the growing demand for interoperability are reshaping how healthcare data is shared. As the industry rapidly evolves, understanding these changes is essential. Embracing innovations helps organizations improve data exchange, streamline workflows, and deliver better patient experiences.
Working with experts from a pharmaceutical software development company can make the transition far less complex. With Relevant Software expertise, providers and payers gain trusted guidance on system evaluations, workflow improvements, and reliable integration strategies. Whether you are planning new HL7 interfaces or moving toward FHIR adoption, our team has the knowledge to help you navigate the process with confidence. Contact us to explore how we can support your next step in digital healthcare.
FAQs
What are the negative aspects of HL7 standards?
While HL7 standards in healthcare improved data exchange, mastering them can be demanding; version drift across sites can be confusing, and local customizations add complexity. Migration costs appear when moving from v2 to FHIR. Careful governance and testing reduce these risks.What are HL7 transmission standards?
HL7 transmission standards define how systems exchange information. Classic messaging covers v2 and CDA over secure transports. Modern programs also use HL7 API standards based on FHIR and REST. Both paths aim for the same goal: interoperable, traceable exchange across platforms.What are the strong security points of HL7 standards?
HL7 healthcare standards promote privacy and integrity through authenticated sessions, in-transit encryption, access control, and audit trails. HL7 FHIR standards pair with SMART on FHIR to scope access and record who saw what. Good practice keeps PHI out of logs and limits data to what a workflow needs.Why are HL7 data standards necessary?
HL7 data standards unify how hospitals, labs, and apps represent information. Consistent fields and codes cut errors, speed handoffs, and support safer decisions. The benefit is simple: the correct data, in the right place, at the right time.Which standards were created by HL7?
HL7 has developed several major standards that define how healthcare data is exchanged: HL7 v2.x, HL7 v3, CDA (Clinical Document Architecture), and FHIR (Fast Healthcare Interoperability Resources). Together, these form the core HL7 messaging formats and API frameworks used throughout the healthcare industry.What are HL7 standards?
Many readers ask, “What are HL7 standards?” It refers to the family of specifications from Health Level Seven that define data structure and exchange. The term HL7 healthcare standards is often used to describe these same rules that guide data exchange between EHR systems, laboratories, and connected applications.What are HL7 API standards?
They are FHIR-based rules for web APIs. Resources such as Patient and Observation travel over REST with predictable search, errors, and paging. SMART on FHIR adds OAuth scopes so apps in an EHR request only the access they need.What is HL7 software and HL7 interface software?
HL7 software includes servers, interface engines, and testing tools that read and write standard messages or u003ca href=u0022https://relevant.software/blog/fhir-resources/u0022u003eFHIR resourcesu003c/au003e. HL7 interface software connects systems, validates content, maps fields, secures transport, and tracks ACKs so teams catch issues early.Do I need HL7 certification?
HL7 certification is optional but helpful. It validates knowledge of core concepts, profiles, and implementation practice. Many teams pair certified staff with robust playbooks, unit tests, and example payloads.Where can I find HL7 documentation?
Official HL7 documentation lives on the HL7 International site and in Implementation Guides for each program. Those guides lock fields, codes, and error behavior, helping partners interpret data consistently.

Hand-selected developers to fit your needs at scale! Let’s build a first-class custom product together.

