The Impact of Electronic Health Records on Healthcare Delivery
Updated: June 4, 2025
We live in a world where healthcare providers can have instant, up-to-the-minute access to patient health histories at their fingertips. Where data-driven insights can guide treatment decisions, and fragmented information does not hinder care coordination. Isn’t it interesting how a single technology – Electronic Health Records – paves the way for such transformation? Yet, what does this digital revolution truly mean for the healthcare sector?
Let’s delve into the impact of Electronic Health Records on healthcare to answer these pressing questions. We’ll explore how far-reaching these transformative changes are – from the individual patient experience to entire medical practices and the broader health ecosystem.

We provide companies with senior tech talent and product development expertise to build world-class software. Let's talk about how we can help you.
Contact usTable of Contents
What Are Electronic Health Records? Brief Exploration
Have you ever thought about how your most recent doctor’s visit was distinct from one you might have had a decade ago? Your doctor probably spent more time clicking and typing than flipping through sheaves of paper. A laptop or a computer screen may have been a permanent fixture in the consultation room, offering immediate access to a plethora of information about your health history. That’s Electronic Health Records (EHRs) at work – a paradigm shift that has discretely yet irrevocably transformed healthcare delivery.

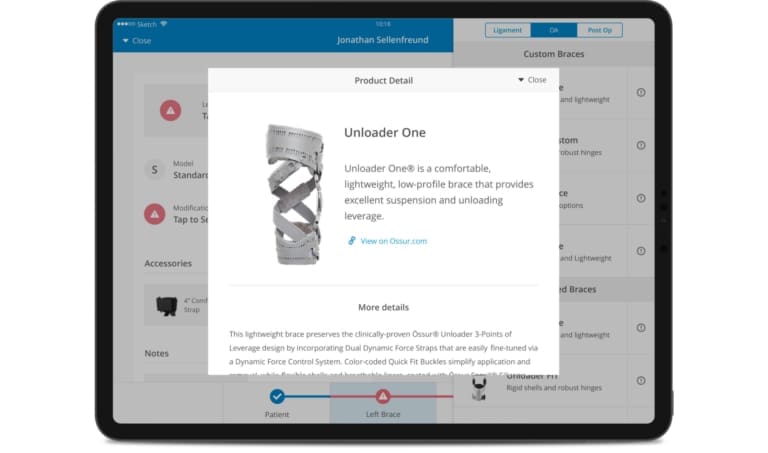
But labeling Electronic Health Records (EHRs) merely as digitized variants of age-old paper medical records is a severe misjudgment of their potential. They are not simply aggregators of medical history, diagnoses, treatments, immunizations, allergies, radiology imagery, or lab results. Instead, EHRs offer a more encompassing perspective of a patient’s health, designed for active, ongoing use, offering continuity of care that paper records can’t match.
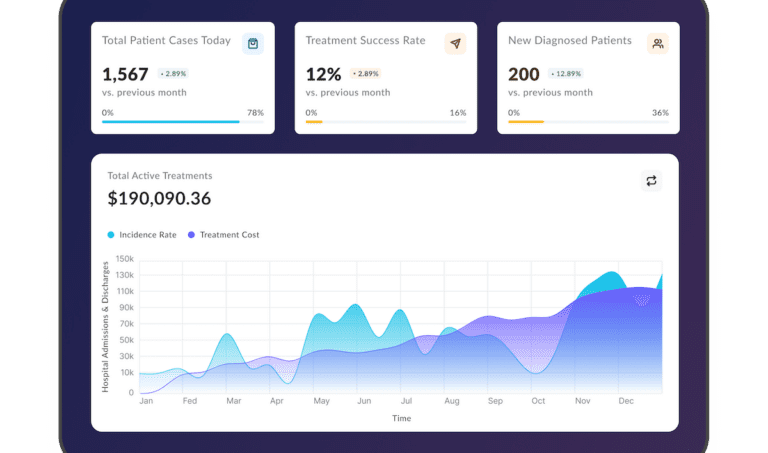
EHRs are real-time, patient-centric databases providing immediate, secure, and comprehensive health details to authorized users across varied healthcare environments. Their core purpose? To refine clinical administrative workflows and establish a more synchronized, efficient healthcare system.
Furthermore, EHRs empower patients, simplifying access to their health data and fostering a more active role in their care. Integrating Artificial Intelligence (AI) and Machine Learning (ML) boosts EHRs’ capabilities, equipping them with predictive analytics to support healthcare professionals in making informed, proactive decisions about patient care.
The Core Components of EHR Systems
The sophistication of Electronic Health Record (EHR) systems lies in their comprehensive suite of features, encompassing multiple components designed to enhance care delivery.
- Patient Demographics: This section holds crucial details like the patient’s name, date of birth, address, contact details, and insurance information. These identifiers are essential for proper patient identification and continuity of care.
- Medical History: The patient’s medical history is recorded meticulously, including chronic diseases, surgeries, allergies, and family medical history, to provide physicians with a comprehensive context during treatment and diagnosis.
- Clinical Data: This section is dynamic and contains all ongoing health information, including doctor’s notes, vitals, diagnoses, medications, and treatment plans. The data from laboratories, radiology, and other diagnostic facilities also fall into this section.
- Medication and Allergy Lists: EHRs keep detailed records of all medications prescribed to a patient, along with dosage, frequency, and duration. Any known allergies to medicines or substances are also noted prominently to prevent adverse reactions.
- Immunization Records: Maintaining an accurate record of patients’ immunization history is crucial, particularly for child and elderly patient populations. These records are necessary for school admissions, international travel, and job requirements.
These components of EHR systems work together, transforming healthcare delivery by improving accuracy, accessibility, and continuity of patient health information.
Essential Functions of EHRs
Electronic Health Records (EHRs) aren’t merely digitized databases of patient information; they offer multifaceted features revolutionizing healthcare delivery. Here’s an examination of EHRs’ principal functions:
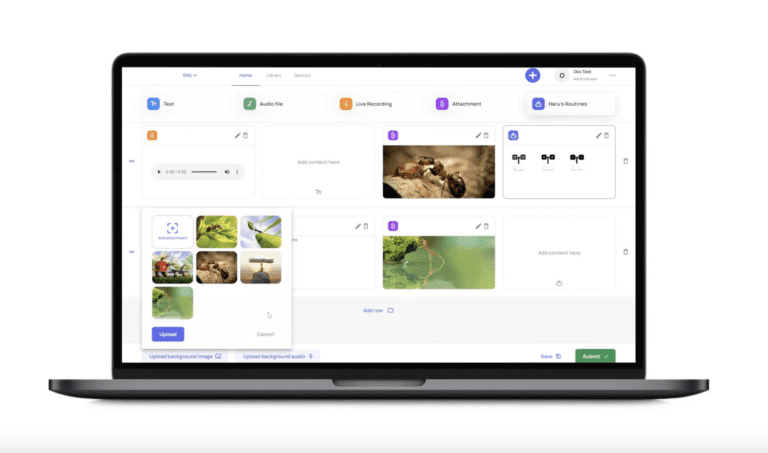
- Data Management: EHRs compile expansive patient data into a singular, readily accessible system. This organized data management bolsters efficiency and productivity in healthcare establishments by providing vital information when required.
- Clinical Decision Support: EHRs come equipped with advanced algorithms for clinical decision support, alerting providers about potential issues such as drug interactions, allergies, and preventive measures. They can even propose diagnosis options, reducing human error and elevating care quality.
- Patient Engagement: Patient portals within EHRs enable enhanced patient interaction. Patients can schedule appointments, request medication refills, examine their medical records, and converse with healthcare professionals. This transparency fosters shared decision-making in healthcare.
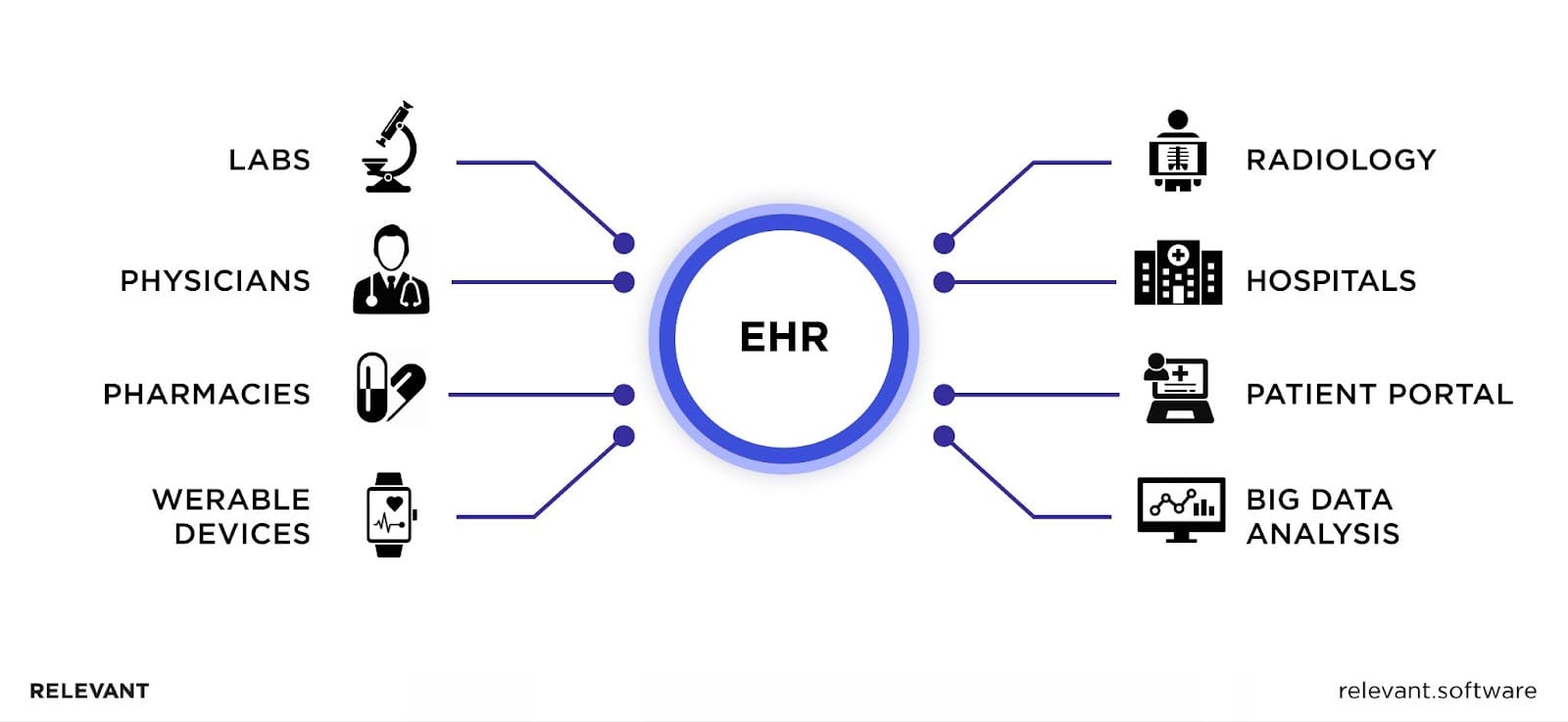
- Interoperability: EHRs ensure smooth data exchange across healthcare environments, including hospitals, clinics, labs, and pharmacies. Such interoperability guarantees that all healthcare providers in a patient’s care access the same exhaustive dataset, promoting better care coordination and continuity.
- Quality Reporting and Improvement: EHRs can track and relay clinical quality measures and public health data. This function aids in performance assessment and benchmarking, contributing to initiatives aimed at quality improvement.
- Billing and Coding: EHRs refine the billing and coding process, reducing errors and assuring accurate reimbursements for services rendered by healthcare providers. This function can enhance revenue cycle management and alleviate administrative pressures.
- Population Health Management: EHRs can spot population health patterns through data analysis, fostering preemptive public health initiatives and efficient resource allocation.
Thus, the functionality of EHRs extends well beyond mere data storage. By boosting data accessibility, fostering patient engagement, assisting in clinical decisions, and enhancing healthcare coordination, EHRs have played a pivotal role in bringing healthcare into the modern age.

Electronic Health Records (EHRs) Vs. Electronic Medical Records (EMRs)
So, what is the difference between EHR and EMR? Both form the backbone of modern healthcare. Yet, they aren’t interchangeable; they depict unique facets of patient data management, each with distinctive functions and advantages.
Essentially, EMRs are the digital version of traditional paper documents. They hold a patient’s medical history, diagnoses, medications, treatment plans, immunizations, allergies, images, and test results from one practice. They allow for data tracking over time, patient monitoring for screenings and check-ups, and verifying patient parameters such as vaccinations and blood pressure.
In contrast, EHRs offer a more comprehensive solution. They exceed the bounds of standard clinical data gathered in a provider’s office, offering a broader patient care perspective. EHRs hold information from all clinicians involved in a patient’s care, including specialists and therapists. They can be securely shared across diverse healthcare settings, resulting in an integrated, real-time, patient-focused record that improves decision-making and patient outcomes.
The difference between EMR and EHR is hidden in the term “health” versus “medical.” While EMRs digitize patients’ medical history, EHRs deliver a comprehensive, holistic view of their health journey. Thus, grasping this difference is pivotal in a healthcare system that increasingly leans on information technology to boost care quality, enhance patient safety, streamline operations, and cut costs.
EMR vs. EHR Comparison Table
| Criteria | Electronic Health Records (EHRs) | Electronic Medical Records (EMRs) |
| Definition | EHRs are comprehensive, patient-centered records that provide a full-fledged view of a patient’s health journey across different healthcare providers and care settings. | EMRs are the digital equivalents of traditional paper charts within a single practice. They offer a concise overview of a patient’s medical history, treatment plans, etc., within one particular healthcare facility. |
| Scope | EHRs compile data from all healthcare professionals engaged in a patient’s care, spanning doctors, specialists, hospitals, labs, and pharmacies. | EMRs typically include information collected within a single provider’s office or clinic. The data may include medical history, diagnoses, and treatments from that particular practice alone. |
| Interoperability | EHRs ensure the confidential, fluid exchange of patient data among varied health professionals. It promotes the integration of health information, improving coordination and continuity of care. | EMRs, in general, lack interoperability capabilities. They are less equipped to share data outside of the individual practice, which can potentially lead to fragmented care. |
| Role in Patient Care | EHRs serve as a valuable tool in facilitating shared decision-making and a patient-centered approach to healthcare. They can improve patient outcomes by offering a more holistic view of their health status. | EMRs serve more of a documentation role, aiding clinicians within a specific practice in tracking patient data over time, identifying patients due for preventive screenings, and managing patients with chronic conditions. |
| Impact on Healthcare Practices | EHRs can streamline administrative tasks, expedite billing and reimbursement processes, support research and data analysis, and facilitate population health management. | EMRs primarily help clinicians diagnose and treat patients effectively within their specific practice by providing a detailed view of a patient’s medical history. They might not significantly influence larger-scale healthcare practices. |
Benefits of Using EHRs in Medical Practice
Electronic Health Records (EHRs) mark a new era in healthcare delivery. This digital evolution has reshaped patient care and healthcare administration. Several of the benefits listed below highlight the impact of electronic health records (EHRs) on the healthcare sector.
Improved Patient Care
EHRs have revolutionized patient care by making health data readily accessible and boosting coordination among healthcare providers. Their comprehensive overview of a patient’s medical history allows personalized treatment plans, improving patient outcomes. This distinction between EHRs and EMRs becomes evident, with EHRs providing a fuller picture of patient health.
Increased Efficiency in Healthcare Practices
EHRs streamline administrative duties, significantly cutting down time spent on paperwork. They help avoid test duplication by giving clinicians access to previous results, saving time and resources. They also speed up billing and reimbursement processes, improving the transparency and effectiveness of financial dealings in healthcare.
Enhancing Data Security
Digital security measures within EHRs offer a higher level of data protection compared to paper records. They also incorporate functionalities for data backup and disaster recovery, ensuring continuous availability and integrity of health data, a crucial aspect in the interoperability of electronic health records.
Facilitating Research and Data Analysis
EHRs have profound implications for research and data analysis. They facilitate population health management, underpinning strategies to improve health outcomes for groups of individuals. EHR integration also plays a critical role in clinical trials and research studies, improving data collection and management. Moreover, monitoring and reporting public health issues become more efficient with EHRs, enabling swift responses to emerging health concerns.
Whether it’s a cloud-based EHR or other types of EHR systems, the impact of electronic health records on workflow, patients, and practices such as pharmacy is indisputable. Comprehending electronic health records’ pros and cons enables healthcare providers to harness them for improved patient care and operational efficiency.
| The impact of electronic health records on workflow | With easy access to patient data, healthcare providers can avoid redundant tests and paperwork. This promotes effective care coordination and timely decision-making, leading to more responsive healthcare delivery. |
| The impact of electronic health records on patients | With these systems, their health information is up-to-date, comprehensive, and easily accessible, leading to personalized and effective treatment plans. EHR incentivizes patient engagement, enabling patients to participate in their healthcare journey actively. |
| The impact of electronic health records on pharmacy practice | EHRs provide pharmacists with complete medication histories, allowing them to manage better and coordinate patients’ medications. This could bolster compliance with drug regimens, mitigate the risk of medicinal cross-reactions, and fundamentally, enhance health results for patients. Additionally, EHRs streamline the prescription refill process and help in medication reconciliation. |
Navigating the Complexities of EHRs
Navigating the complexities of Electronic Health Records (EHRs) involves numerous challenges, from initial implementation costs to concerns over data privacy and overcoming interoperability and data sharing issues.
Implementation Costs
One cannot discuss EHRs without acknowledging the hefty financial investment that comes with its adoption. The initial outlay for procuring and installing these systems is often substantial, causing significant strain on the financial resources of healthcare organizations. Furthermore, the cost of EHRs is not a one-time expenditure. Ongoing expenses for maintenance, software upgrades, and troubleshooting are inevitable components of EHR use.
In addition, the complexity of EHRs necessitates comprehensive staff training to ensure efficient workflow, reducing the likelihood of errors that could impact patient care. Thus, while EHRs can improve efficiency and patient outcomes, their implementation may demand significant cost and time investment.
Data Privacy and Security Risks
EHRs’ digital nature, while bringing benefits of accessibility and ease of sharing, also introduces data privacy and security risks. Data breaches can have catastrophic consequences, including patient mistrust and legal repercussions. Compliance with critical laws such as the Health Insurance Portability and Accountability Act (HIPAA) and the General Data Protection Regulation (GDPR) is crucial. Yet, it adds another layer of complexity to the EHR landscape.
Electronic Health Records need robust security measures that effectively shield sensitive patient data while simultaneously allowing necessary access to healthcare providers. Navigating this fine balance is indeed a daunting yet fundamentally crucial task when dealing with the complexities of EHRs.
Interoperability and Data Sharing
EHRs harbor the potential to integrate and unify disparate healthcare systems; however, the fulfillment of this promise has been slow due to interoperability issues. These systems often struggle to communicate effectively, leading to fragmented data and obstructed information flow. Such complications hinder the seamless exchange of patient information between healthcare providers, impacting workflow, patient care, and pharmacy practice.
Moreover, implementing interoperable standards (like FHIR) is a laborious process involving many stakeholders. It demands technical expertise, the ability to reach a consensus, and an investment of time and resources. Until this challenge is adequately met, the full potential of EHRs will remain untapped.
Nevertheless, with thoughtful planning and efficient management, the potential benefits of EHRs can greatly outweigh these obstacles. Especially if you involve proficient healthcare software development partners to implement this tool in your healthcare practice.
Sum It Up
Electronic Health Records signify a transformative shift in healthcare delivery. Yet, successful EHR integration necessitates careful navigation of challenges, including cost considerations, data privacy and security risks, and interoperability issues.
Our proficiency in healthcare IT consulting and web development is invaluable in this context. We are adept at addressing EHR implementation costs, minimizing them through strategic planning, and maximizing your return on investment.
As for privacy and security, we prioritize data protection above all else. We ensure our EMR systems comply with stringent regulations such as HIPAA and GDPR. Our robust security frameworks shield against data breaches, fostering trust between you and your patients.
Finally, we excel at resolving interoperability issues. Our HL7 FHIR Implementation Services guarantee seamless data exchange, integrating disparate healthcare systems into a cohesive whole. This approach aids in promoting collaborative, holistic patient care and amplifying operational efficiencies.
Why merely adapt when you can transform? Contact us and let our healthcare software development team steer you toward innovative solutions. Also, read about Metaverse in Healthcare and how it will reshape the industry.
FAQ
Our core services:
Do you want a price estimate for your project?
Do you know that we helped 200+ companies build web/mobile apps and scale dev teams?
Let's talk about your engineering needs.
Write to us