In-Depth FHIR Implementation Guide: Understanding Healthcare Interoperability
Updated: June 4, 2025
Healthcare data interoperability has shifted from optional to crucial for improving patient care, outcomes, and system efficiency. Fast Healthcare Interoperability Resources (FHIR) stands as a vital instrument catalyzing this paradigm shift in healthcare data exchange.
Consequently, gaining a command of FHIR’s capabilities and facilitating its seamless operation is becoming an unignorable responsibility for healthcare providers, software developers, and IT specialists aiming for software integration.

We provide companies with senior tech talent and product development expertise to build world-class software. Let's talk about how we can help you.
Contact usIn light of this, we present an exhaustive FHIR implementation guide – an essential reading for stakeholders of data interoperability in healthcare. This guide clarifies FHIR’s meaning, highlights its significant deployment advantages, and provides a detailed roadmap for its execution – an indispensable tool for transforming healthcare delivery.
Table of Contents
What is FHIR in Healthcare?
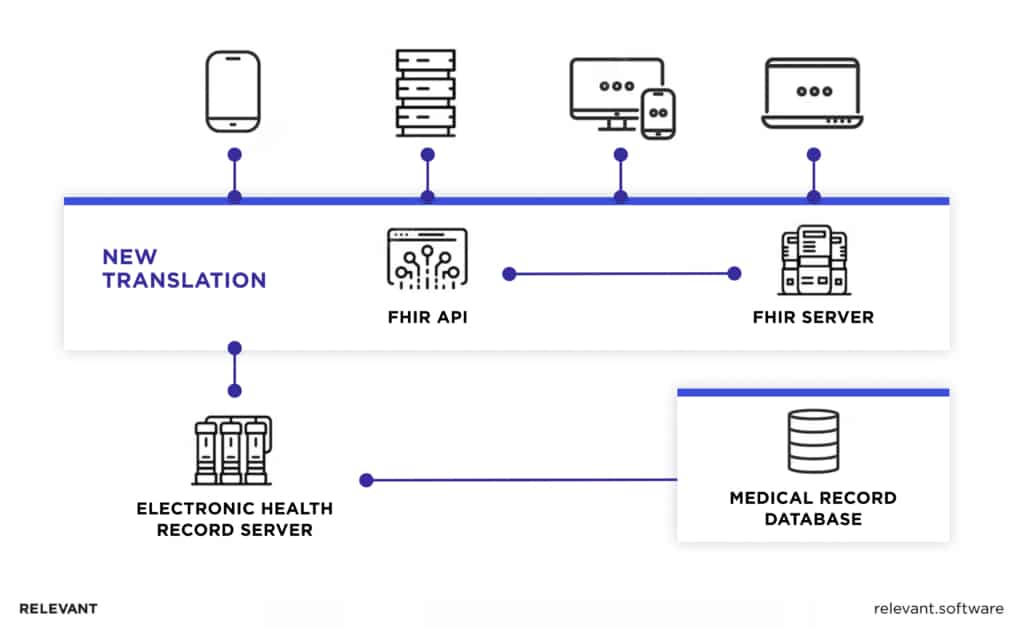
Fast Healthcare Interoperability Resources, or FHIR, symbolizes a groundbreaking evolution in the administration and transfer of healthcare data. It is an open, standardized framework developed by Health Level Seven International (HL7), designed to improve the exchange of healthcare information between providers and patients, leveraging familiar web standards.
For healthcare professionals, FHIR can be seen as the cornerstone of health data interoperability. It simplifies the sharing of health data across different health systems, effectively breaking down data silos, and allowing caregivers to have a more holistic view of their patient’s health status. This yields enhanced patient healthcare and superior treatment results.

From an IT professional’s perspective, FHIR presents a model that utilizes well-known web standards such as RESTful APIs, XML, and JSON for data formats and OAuth for authentication. These known standards make it easier to implement, unlike previous health data standards that required specialized knowledge.
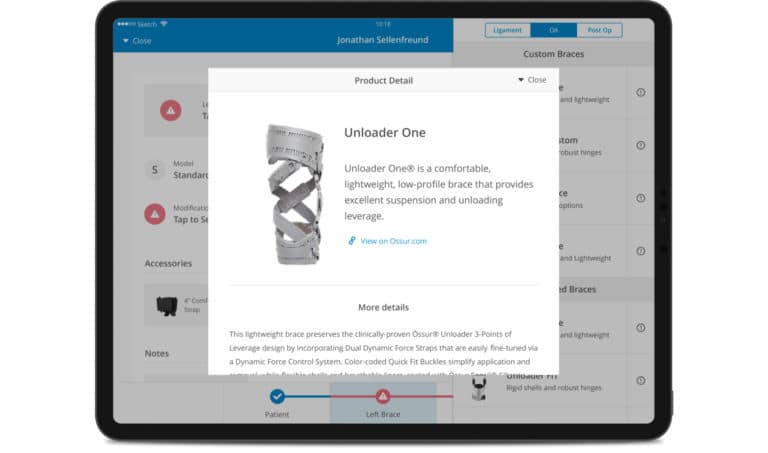
Software developers working in healthcare can appreciate FHIR’s modularity and flexibility. FHIR is based on the concept of “Resources,” which are discrete chunks of data that can be worked with independently or can be combined to build complex documents. This structure allows developers to use as much or as little of the FHIR standard as they need, streamlining the development process.
Lastly, for stakeholders involved in healthcare data exchange and interoperability initiatives, FHIR provides a way to drive real-world improvements in healthcare quality and efficiency. The adoption of FHIR can result in more informed clinical decision-making, increased patient engagement, enhanced data security, and cost-effective healthcare data management. In essence, FHIR is more than just a data standard; it is a tool that can transform the very foundation of healthcare delivery.
Benefits of Implementing FHIR
Implementing Fast Healthcare Interoperability Resources (FHIR) yields a wealth of benefits that remodel healthcare operations, fostering an environment of enhanced patient care and system efficiency.
- Arguably, the most profound benefit of FHIR is interoperability. It allows disparate healthcare systems to communicate with each other seamlessly, eliminating data silos and facilitating the secure exchange of health information. Whether it’s a hospital, a clinic, a lab, or a pharmacy, all can share and access critical patient information with ease, leading to more coordinated and efficient care.
- Improved patient engagement is another significant boon. With FHIR, patients can have more access to and control over their health data, leading to increased participation in their care process. This involvement boosts patient satisfaction and has the potential to improve health outcomes.
- FHIR’s use of standardized, modern web technologies allows for easier and more cost-effective implementation. It utilizes well-known technologies, such as RESTful APIs, XML, and JSON, significantly reducing the learning curve and implementation costs compared to older healthcare data standards.
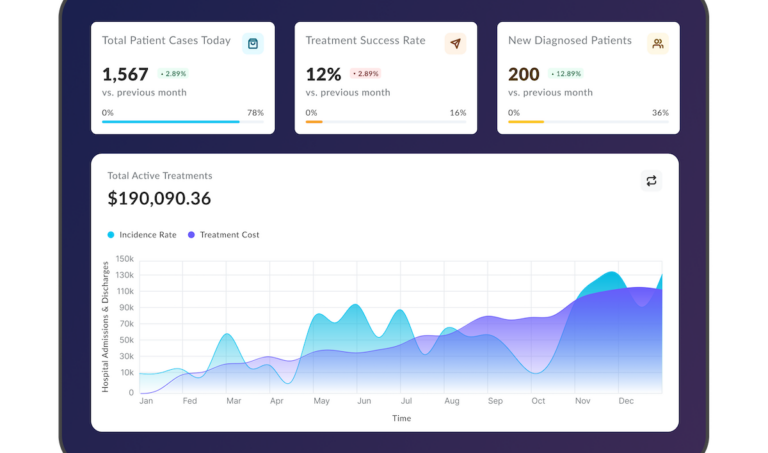
- In addition, FHIR aids in real-time, data-driven decision-making. It enables healthcare providers to access up-to-date patient data, leading to informed clinical decisions. This can lead to improved patient outcomes, decreased hospital readmissions, and more effective preventive care.
- Finally, FHIR implementation aids in healthcare research by facilitating the exchange of research data, making it easier for researchers to find patterns, test hypotheses, and make discoveries that can lead to better treatments and cures.
In a nutshell, FHIR implementation not only optimizes healthcare operations and patient care but also contributes to reducing costs, enhancing research, and ultimately transforming the healthcare industry. Its implementation is an investment that yields significant returns, leading to a more interconnected and effective healthcare ecosystem.
Your Next Read: Digital Twin in Healthcare
The Most Common Approaches of FHIR Implementation
Fast Healthcare Interoperability Resources (FHIR) is a flexible framework that offers multiple implementation options tailored to the distinct requirements of healthcare organizations. The four most common approaches to FHIR implementation are:
1. FHIR RESTful API Implementation
In a RESTful API implementation, FHIR leverages web standards to create, read, update, and delete (CRUD) operations on resources. This approach is particularly valuable in real-time applications where healthcare systems need to interact dynamically. It’s a straightforward method where resources are treated as URLs, and standard HTTP verbs are used. RESTful API implementation is popular because of its simplicity, scalability, and compatibility with modern web architectures.
2. FHIR Messaging Implementation
In the messaging implementation, FHIR resources are used within existing HL7 message structures. This allows healthcare systems to take advantage of FHIR’s granularity and flexibility while retaining their investment in HL7 messaging infrastructure. It’s an event-driven model, where a trigger event in one system leads to a message being sent to another system. This approach is suitable for batch-style and background processing tasks.
3. FHIR Document-Based Implementation
In the document-based implementation, FHIR resources are bundled together to create self-contained, discrete units of healthcare information called documents. This is a particularly effective way to handle complex use cases that involve multiple resources, such as a discharge summary or a referral note. These documents can then be readily shared, stored, and retrieved, making them ideal for interoperability purposes.
4. FHIR Hybrid Implementation
As the name suggests, hybrid implementation combines various approaches based on the healthcare system’s needs. For example, a healthcare provider could leverage a RESTful API to facilitate real-time interactions, utilize messaging for batch processing tasks, and employ document-based approaches for handling complex FHIR use cases. This flexible approach ensures that healthcare systems can leverage FHIR’s strengths in a way that best suits their operational needs and strategic goals.
Choosing the right approach for FHIR implementation requires a careful understanding of the healthcare system’s requirements, existing infrastructure, and strategic goals. With the right approach, FHIR can significantly enhance healthcare data interoperability, leading to improved patient care and operational efficiency.
FHIR Implementation Challenges
Implementing Fast Healthcare Interoperability Resources (FHIR) holds significant promise for enhancing healthcare data interoperability. However, like any significant technological shift, it brings a unique set of challenges that must be addressed for successful implementation.
Data Security and Privacy Concerns
The expanded data exchange capabilities of FHIR bring forth legitimate considerations regarding the security and privacy of sensitive patient data. Balancing the imperative of safeguarding patient information with the facilitation of interoperability poses a significant challenge. Healthcare organizations must implement robust security protocols, including secure data transmission and storage, and manage patient consent effectively.
Legacy System Integration Challenges
Many healthcare organizations rely on legacy systems for their day-to-day operations. Integrating these systems with FHIR, which is based on modern web standards, can be challenging. Overcoming this hurdle often involves significant transformation work and potential disruptions, requiring meticulous planning and strategic resource allocation.
Standardization and Semantic Interoperability Issues
While FHIR provides a standard for data exchange, differences in data definitions and interpretations can still create issues, referred to as semantic interoperability challenges. Ensuring that all systems understand and interpret the data, in the same way, is a key challenge. This requires a shared understanding and agreement on the meaning and use of data.
Governance and Organizational Readiness
Implementing FHIR is not just a technological change but an organizational one. It requires the development of new governance structures to manage data sharing, ensure compliance with regulations, and resolve potential disputes. Furthermore, organizations need to assess their readiness for change and ensure buy-in from stakeholders at all levels. This involves considerable change management efforts to align people, processes, and technology.
Notwithstanding these obstacles, the substantial advantages of implementing FHIR in elevating healthcare data interoperability, enhancing patient outcomes, and optimizing operational efficiency are profound. Tackling these challenges proactively through meticulous strategic planning, effective governance, and robust leadership will lay the groundwork for a triumphant journey in implementing FHIR.
FHIR Implementation: Step-by-step Guide
Implementing FHIR requires meticulous planning and execution. By fully embracing this comprehensive, step-by-step guide, you will gain the essential knowledge and strategies required to harness the complete potential of FHIR.
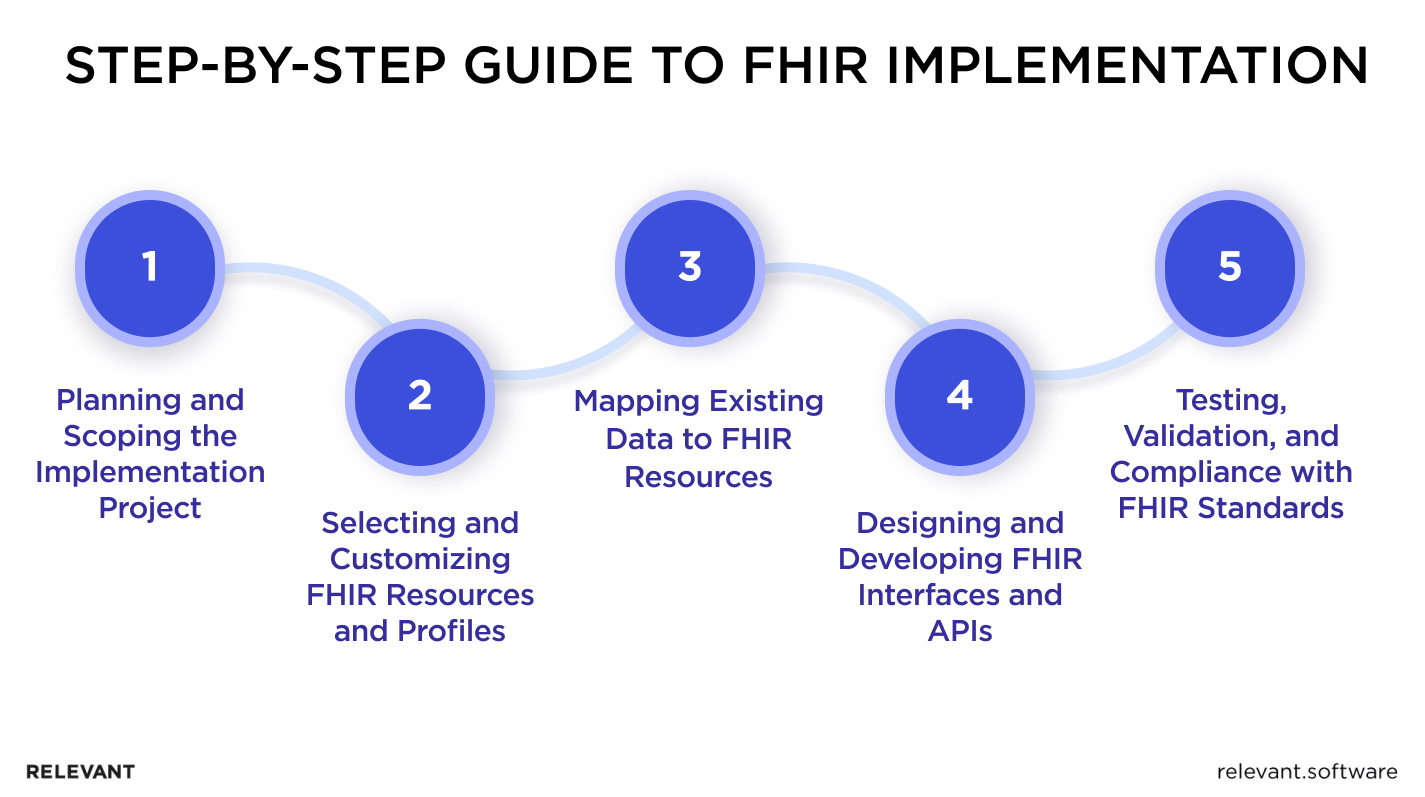
Planning and Scoping the Implementation Project
The success of any project lies in meticulous planning and well-defined scope. First, establish clear objectives. What do you aim to achieve with FHIR? Is it enhancing interoperability, improving patient data management, or both? Understanding the objective will help you define the scope. Also, identify key stakeholders, allocate resources, and develop a realistic timeline. Create a risk management strategy to address potential challenges and ensure seamless execution.
Selecting and Customizing FHIR Resources and Profiles
FHIR is based on modular components called “Resources.” Each resource caters to a specific type of data (like a patient, practitioner, or appointment). Identify the resources relevant to your requirements and customize them accordingly. Understanding the FHIR profiles, which are customizations of resources, will allow you to adapt them to suit your needs and comply with regional healthcare standards.
Mapping Existing Data to FHIR Resources
The next step is to map your existing data to the selected FHIR resources. This involves transforming and standardizing the existing health data into the FHIR format. It’s crucial to ensure data integrity during this process to preserve its quality and utility. Careful planning, including deciding which data to map and determining how to handle complex data structures, will be essential here.
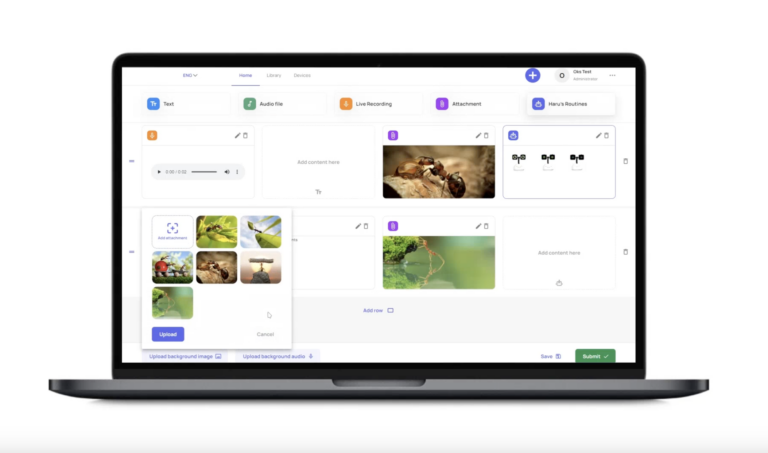
Designing and Developing FHIR Interfaces and APIs
Developing FHIR APIs and interfaces involves creating software interfaces that enable healthcare systems to exchange data using FHIR standards. This process requires deep knowledge of RESTful API principles and common data formats like XML and JSON. The design should be user-friendly and robust, ensuring data security and allowing seamless interaction with other systems.
Testing, Validation, and Compliance with FHIR Standards
The final step involves testing the implementation for functionality and performance. Validate whether the system is correctly utilizing FHIR resources, managing patient data, and communicating with other systems. Confirm your system’s compliance with relevant regulations, standards, and best practices. Any non-compliance or error should be addressed and rectified immediately to ensure a robust, reliable, and interoperable FHIR implementation.
This step-by-step guide, when followed rigorously, will lead you to a successful FHIR implementation, ushering in a new era of enhanced interoperability in your healthcare setting.

How expensive is FHIR development?
The cost of FHIR development hinges on crucial factors that shape project planning and resource allocation. Grasping these determinants is vital for precise budgeting and ensuring the triumphant execution of FHIR initiatives. Let’s delve into these key factors briefly:
- Scope and Complexity: Projects with extensive functionality, intricate data models, or sophisticated integration requirements may necessitate additional resources, development time, and specialized expertise, thereby driving up the overall cost.
- Interoperability Requirements: The level of interoperability required for your specific project can affect complexity and cost. Integrating with multiple systems, ensuring data consistency, and adhering to industry standards may incur additional expenses.
- Data Volume and Complexity: Projects dealing with large data sets, complex data transformations, data mapping, and data validation requirements may require extra development effort and resources, thereby impacting the overall cost.
- Integration and Customization: FHIR development often involves integrating with existing systems and customizing FHIR resources and profiles to align with specific requirements. This can affect development efforts and subsequently impact the cost.
- Security and Compliance: Incorporating robust security controls, adhering to privacy regulations (such as HIPAA), and implementing comprehensive audit trails can add complexity and cost to the development process.
- Development Team Expertise: Highly skilled developers with in-depth knowledge of FHIR standards and healthcare domain expertise may come at a higher cost. However, their proficiency can contribute to smoother development and better outcomes.
- Project Timeline: Projects with rushed or accelerated timelines may require additional resources or overtime, potentially increasing the expenses.
To get a more accurate estimate of the costs of your FHIR solution, we recommended consulting with our experts in FHIR implementation. They can assess your organization’s specific needs, evaluate the project’s scope, and provide insights tailored to your situation.
Best Practices of FHIR Implementation
Implementing FHIR is a significant undertaking, and adopting the following best practices can streamline the process and ensure successful outcomes.
- Engaging Stakeholders and Fostering Collaboration. FHIR implementation affects various stakeholders within an organization, including clinicians, IT staff, administrators, and patients. Engaging these stakeholders from the outset fosters a collaborative environment, ensures their needs are considered, and increases buy-in for the project.
- Adhering to FHIR Implementation Guides and Standards. The use of standard FHIR resources and profiles, as outlined in the FHIR implementation guides, is crucial. These guides offer proven techniques and established practices crafted by industry authorities. They guarantee uniformity, seamless data exchange, and adherence to regulatory requirements.
- Conducting Thorough Testing and Validation. This includes checking that the system correctly uses FHIR resources, communicates with other systems as intended, and complies with security standards. Regular testing and validation help to identify and address issues early, ensuring the robustness and reliability of the implementation.
- Ensuring Ongoing Support and Maintenance. FHIR implementation is not a one-time activity. It requires ongoing support and maintenance to ensure it continues to meet the organization’s needs, remains secure, and keeps up with updates to the FHIR standard and regulatory environment. This includes regular reviews, updates, and training for users.
Bottom Line
FHIR implementation paving the way for enhanced interoperability, improved patient outcomes, and operational efficiency. Though it presents challenges, with the right planning, adherence to best practices, and a strategic approach, FHIR’s benefits can be fully realized.
Considering the magnitude of the task, adopting interoperability can be daunting if you’re venturing into it for the first time. Fortunately, you can delegate this undertaking to a third-party service provider like Relevant – an outsourcing software development company specializing in healthcare interoperability initiatives.
Our pool of seasoned software engineers boasts extensive experience in adopting HL7 standards, with a special focus on HL7 FHIR Service. These experts can provide assistance on particular tasks or assume complete control over your project, depending on your unique requirements. In essence, Relevant Software can:
- Provide you with expert healthcare consultancy on achieving FHIR interoperability, grounded in thoroughly analyzing your current system.
- Augment your workforce by offering our healthcare software development engineers to aid with practical tasks like system optimization or integration.
- Assemble a dedicated team that will construct interoperable systems from the ground up, tailored to your needs.
Contact us today to discuss your specific needs and embark on a transformative journey toward seamless healthcare data exchange and improved patient care.
FAQ
Our core services:
Do you want a price estimate for your project?
Do you know that we helped 200+ companies build web/mobile apps and scale dev teams?
Let's talk about your engineering needs.
Write to us