Machine Learning in Healthcare: A Step-by-Step Implementation Guide with Real Cases

At a London hospital, a patient comes in with chest pain. His tests look normal, so under usual circumstances, he would be sent home. But an AI system spots subtle warning signs of a possible cardiac event. Doctors act fast, perform a procedure, and save his life. That’s how machine learning in healthcare changes outcomes.
This technology prevents misdiagnoses, detects cancer earlier than specialists, predicts outbreaks before they spread, and accelerates drug discovery. The impact shows up in accuracy, speed, and patient outcomes.
from 25 countries outsourced software development to Relevant
We provide companies with senior tech talent and product development expertise to build world-class software.
Still, adoption isn’t easy. Hospitals face fragmented data, strict regulations, and outdated systems that don’t communicate with one another. Many AI projects fail here, not because the models don’t work, but because there’s no clear way to bring them into daily clinical use.
So, what works in practice? This guide maps a step-by-step route from concept to clinic, grounded in Relevant Software’s delivery experience. It covers use cases, data strategy, model validation, deployment, and change management, in the same steps used in our AI development services.
What is machine learning in healthcare: definition and key concepts
Machine learning in healthcare is a branch of AI that enables systems to learn from data and improve over time. Unlike traditional code that follows fixed rules, ML models infer patterns from examples and predict outcomes for new cases. The result is faster insight, fewer errors, and support for informed clinical decision-making.
Core types of ML
Machine learning in healthcare relies on three learning modes that solve different problems. Each mode suits a different data shape, label quality, and workflow.
- Supervised learning. Models train on labeled examples with known answers. Teams use it to predict disease risk, flag abnormal labs, prioritize medical imaging studies, or recommend therapies based on prior outcomes.
- Unsupervised learning. Models analyze unlabeled data to reveal structure. In healthcare, it helps identify new patient phenotypes, detect previously unknown disease clusters, and find subtle signals in medical images or EHR data. These insights often enhance later machine learning models and lead to more precise diagnostics and treatments.
- Reinforcement learning. An agent learns by trial, feedback, and reward. In care pathways, it can optimize dosing schedules, order sets, and ICU interventions under clear safety rules so clinicians stay in control.
Machine learning algorithms and healthcare use
Artificial intelligence turns health data into decisions across clinical practice, clinical trials, and care delivery. AI models process electronic health records, medical images, and patient data, understand natural language in clinical notes and discharge summaries, and enable large-scale precision medicine.
By combining big data, predictive analytics, computer vision, and natural language processing, healthcare providers gain sharper insights for clinical decision support. At the same time, data scientists and healthcare organizations ensure that AI models remain accurate, compliant, and truly beneficial for each patient.
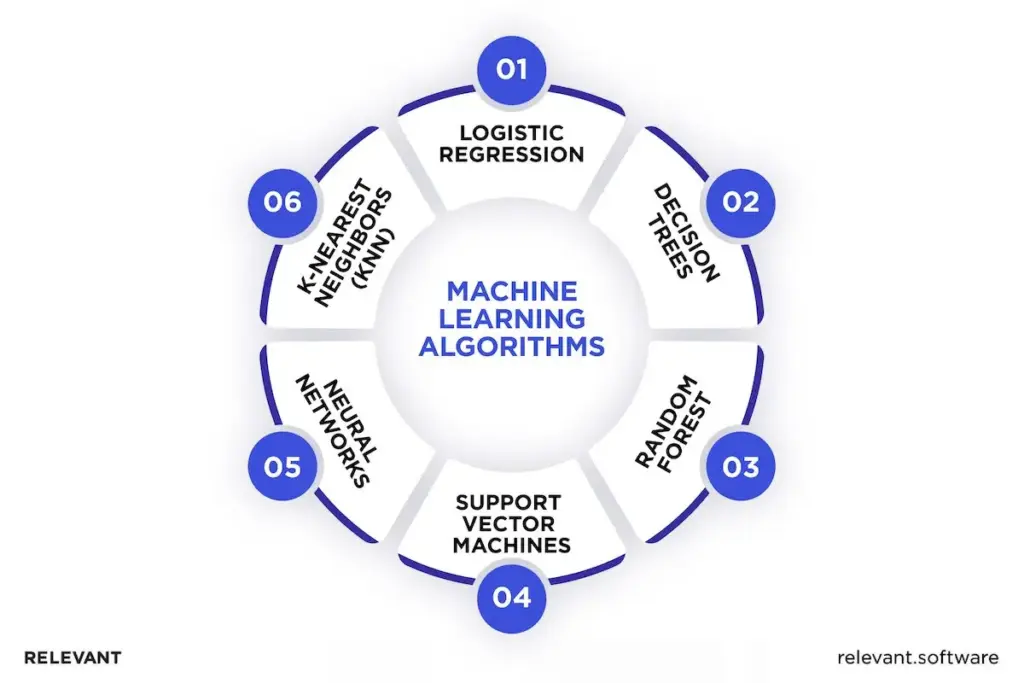
Logistic regression
A fast, reliable baseline for yes/no outcomes.
Use for: disease risk scoring in chronic conditions, predicting hospital readmissions from EHR timelines, and identifying epidemiological associations across large datasets.
Decision trees
Easy to interpret, with transparent rules that clinicians can review and audit.
Use for: mapping symptom-to-diagnosis flows, selecting cancer treatments, flagging complication risks in high-risk groups, and checking data entry quality.
Random forest
This method uses many decision trees that work together and “vote” on the result. Because it combines multiple opinions, it’s more accurate and less sensitive to errors or missing data.
Use for: predicting patient outcomes, finding the most important health factors, and forecasting hospital resources such as beds or supplies.
Support vector machines (SVMs)
Excel at finding clear boundaries in high-dimensional data.
Use for: classifying cancer subtypes from medical images or genomic data, stratifying patient risk based on history, and segmenting tumors in imaging.
Neural networks
Deep models that capture complex relationships in images, text, and time-series data.
Use for: computer vision in radiology and ophthalmology, pathology slide analysis, NLP on clinical notes, decision support from longitudinal EHRs, and discovering signals in drug development.
K-nearest neighbors (KNN)
Simple, case-based reasoning that effectively detects similarities and anomalies.
Use for: patient similarity searches, early warnings from vital-sign changes, small-cohort classifiers in clinics, and spotting outliers in clinical trials.
Why machine learning matters in healthcare
Hospitals generate oceans of patient data: EHR notes, lab results, device streams, and medical imaging. Much of it sits in silos or unstructured files. A modern machine learning model turns that raw input into a usable signal that improves patient health and quality of care across the healthcare system.
NLP pulls facts from clinical notes. Computer vision reads scans. Thoughtful feature extraction and data analytics link timelines across encounters. Together, these ML systems power predictive models that flag high-risk patients, surface relevant medical history, and deliver real-time clinical decision support.
A data-driven industry that cannot use its own data
As we mentioned above, most health care data is unstructured, which makes it hard to search, join, and analyze at scale. Data collection has surged in recent years across digital health and devices, yet many organizations still struggle to unlock value. Machine learning applications change that.
Deep learning and natural language methods extract signals from imaging, genomics, EHR notes, and wearable streams. The payoff is earlier detection of medical conditions, sharper risk stratification, and treatment plans tailored to individual patients rather than population averages.
Beyond human limits: accuracy, speed, precision
In mammography, AI helps detect more true cases of cancer while reducing false alarms. In sepsis care, early-warning systems alert clinicians sooner, leading to faster treatment and lower mortality. In dermatology, AI models flag suspicious skin lesions, giving specialists an extra layer of support. Across research on Google Scholar, the same conclusion appears: machine learning strengthens human intelligence — it doesn’t replace it.
The cost factor: less waste, real savings
Machine learning also improves operations. Analytics-led scheduling and command centers reduce access delays and raise throughput. Health systems have reported shorter wait times after centralizing scheduling and applying business intelligence to capacity planning. The result is fewer bottlenecks, smoother care delivery, and measurable value for providers and patients.
Your next read – Benefits of AI in healthcare
Examples of machine learning in healthcare
Below are real examples of machine learning in healthcare today. Each case shows a practical application that helps answer real clinical questions and supports day-to-day medical decisions.
- Sepsis early warning. Machine learning models combine vitals, labs, and clinical notes to estimate the near-term risk of deterioration. The alerts appear in the EHR, giving rapid-response teams time to act. Hospitals using these systems report faster antibiotic delivery and lower mortality rates in critical care units.
- Diabetic retinopathy screening. Computer vision analyzes retinal photographs from fundus cameras and automatically grades disease severity. Cases that require specialist review are flagged and routed to ophthalmologists. This approach allows screening to expand into primary care and helps detect vision-threatening conditions earlier.
- Radiology triage. Image classifiers score chest X-rays and CT scans for urgent findings such as pneumothorax or pulmonary embolism. The radiologist’s worklist reorders automatically, so critical studies move to the top. The result is shorter turnaround times for high-risk cases without slowing down routine imaging workflows.
- Readmission risk prediction. Predictive models draw on prior admissions, comorbidities, medications, and social factors to estimate the likelihood of a patient returning within 30 days. Care teams use these insights to prioritize follow-up appointments, home visits, and support programs, reducing avoidable readmissions and easing pressure on bed capacity.
- Trial cohorting. Natural language processing and rule-based filters scan patient records against trial inclusion and exclusion criteria. Coordinators receive candidate lists with supporting evidence, which speeds up recruitment and lowers screen-fail rates. As a result, clinical trials move faster and patients gain earlier access to new therapies.
The next question is execution. How does an organization implement applications of machine learning without waste or stalled pilots?
Step-by-step guide to implementing machine learning in healthcare
Machine learning in healthcare delivers results only with disciplined execution. Technology does not win on its own. Strategy, compliance, and clean integration decide impact.
Relevant Software experts outline six steps that turn AI spend into better outcomes, higher efficiency, and measurable value.
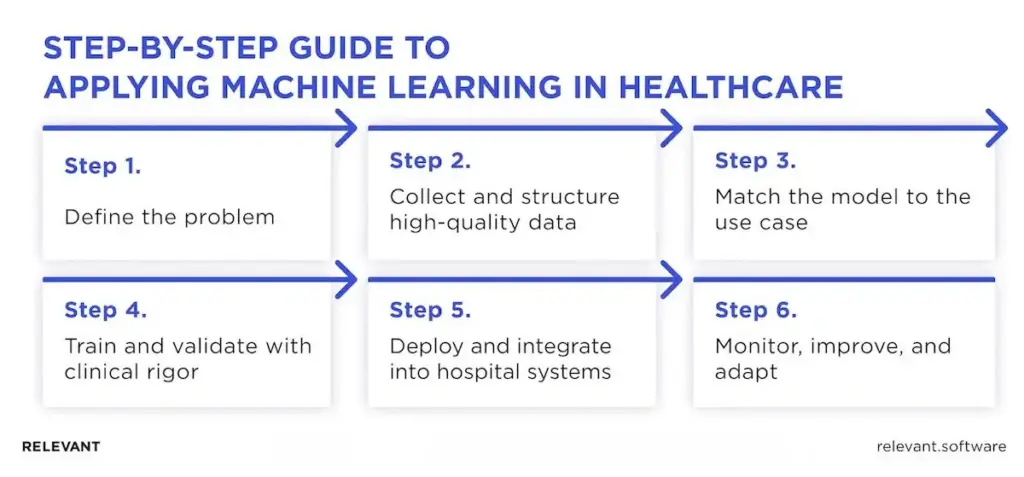
Step 1: Define the problem
Start with one clear, measurable goal — assign an owner, a baseline, and a deadline.
- Clinical: reduce misdiagnoses, increase diagnostic accuracy, or improve early detection.
- Operations: lower readmissions, improve patient flow, or optimize bed and theatre use.
- R&D: shorten clinical trial cycles, refine cohorts, or detect stronger safety signals.
Vague goals stall progress. Specific metrics drive results. For Relevant Software clients, these targets are documented in a decision brief before any model development begins.
Step 2: Collect and structure high-quality data
Reliable, well-organized data is the backbone of any successful machine learning project. The team identifies all relevant sources, such as electronic health records, imaging systems, lab results, genomic databases, medical devices, and clinical trial datasets, and ensures quality by removing duplicates, aligning medical codes, standardizing units, and tracking data lineage. Privacy and compliance come next, with de-identification, access control, and audit trails that meet HIPAA and GDPR standards.
Interoperability is also key. Using FHIR protocols and vendor APIs helps reduce manual work and ensures smooth data exchange. In cases where data cannot leave a hospital, federated learning enables models to train locally, sharing only updates rather than raw data.
Step 3: Match the model to the use case
Once the data is ready, the right modeling approach must be selected. Supervised learning is best suited for tasks such as diagnosis, triage, or risk scoring. Unsupervised learning helps uncover new patient phenotypes or disease clusters. Reinforcement learning can guide treatment planning, provided strict clinical safeguards are in place.
The choice of algorithms also depends on the data type. Medical images benefit from convolutional neural networks or vision transformers. Clinical notes are better handled with NLP models built on medical ontologies. Tabular EHR data works well with gradient boosting or logistic regression as a strong, interpretable baseline.
Step 4: Train and validate with clinical rigor
We train and test models to ensure they deliver results clinicians can trust. Data is split for fair evaluation, and we measure accuracy, sensitivity, and specificity to confirm performance. Each prediction includes a confidence score, and we check for bias across patient groups and devices. All experiments, datasets, and outcomes are documented to ensure full transparency and reproducibility.
Step 5: Deploy and integrate into hospital systems
We deploy AI models directly into clinical environments where decisions are made. It connects directly to electronic health records and other hospital systems, so doctors don’t need to switch between tools. The model explains its reasoning clearly and visually, helping staff understand each suggestion. Every decision is tracked for safety, and the system always follows medical regulations. If the model isn’t confident, it automatically defers to standard clinical procedures.
Step 6: Monitor, improve, and adapt
We continuously track how the model performs in real-world conditions. Our team monitors accuracy, data changes, and clinical results to spot any early drop in performance. Updates are released regularly under strict control, with the option to roll back if needed. We gather feedback from clinicians to ensure improvements deliver real value at the bedside. After every update, we review security and compliance to ensure patient data remains fully protected.
For a deeper dive into best practices, explore our insights on machine learning development.
These steps are based on Relevant Software’s real-world work with healthcare organizations. We ensure AI systems stay accurate, compliant, and clinically effective, so investments translate into real improvements in patient care and operations.
Barriers and challenges to machine learning adoption in healthcare
Of course, implementing machine learning in healthcare isn’t without its challenges. Based on Relevant Software experience, the biggest hurdles cluster around messy data, EHR integration, bias and fairness, safety with transparency, regulatory approval, scarce talent, and proof of ROI. The sections below unpack each issue and show clear steps that help teams move from pilot to safe, trusted use at scale.
Data quality
Machine learning is only as reliable as the data behind it. In healthcare, data integrity is a constant challenge. Hospitals use different coding systems, lab measurements vary by region, clinical notes include free text that’s hard to standardize, and duplicates appear in nearly every dataset. These inconsistencies distort labels, hide meaningful patterns, and weaken predictions — right where clinicians need accuracy most. Without clean, well-managed data pipelines, even the strongest model design fails to deliver trustworthy results.
Expert tip: Standardize medical terms and measurement units, remove duplicate records across systems, run structure and range checks, and track where every data point comes from. Never start model training until all data validation checks are complete.
Patient consent
Using personal health information (PHI) without proper permission poses significant legal and ethical risks. Clinicians need data to diagnose and treat patients, but patients ultimately control how their information is used. Consent rules vary by country, organization, and even hospital, and outdated forms often create compliance gaps uncovered during audits. For machine learning in healthcare, every dataset must be tied to documented, auditable patient consent.
Expert tip: Always collect explicit consent, record and audit every data access, respect withdrawal requests, anonymize information whenever possible, and maintain clear, transparent data-access policies.
Safety and transparency
Doctors hesitate to act on answers they cannot inspect, and regulators do the same. Safety means consistent performance across patient groups and care sites, with clear limits on use. Transparency means each result shows key drivers, a short rationale, and calibrated confidence. Without this context, trust and adoption stall.
Expert tip. Favor interpretable models when possible. For complex models, provide faithful explanations, calibrated confidence intervals, and references to relevant evidence or guidelines. Publish a brief model card with data scope, known limits, and a plan to monitor performance. Test across sites, keep audit logs, and leave final decisions with clinicians.
Data privacy and security
Medical data is one of the most valuable and vulnerable assets in the world. A single breach can cause lasting harm to patients, staff, and the institution. Protecting it isn’t just about compliance; it’s about maintaining trust. From storage to transmission to access, every step must be secured and auditable.
Expert tip. Apply federated learning to keep data on hospital premises, use end-to-end encryption for both transit and storage, enforce zero-trust access with strict permissions, and run automated compliance checks for HIPAA, GDPR, and FDA.
Bias and ethical concerns
When the data used to build an AI tool does not match the patients it will serve, the tool can favor some groups and miss others. A model trained mostly on adult records may overlook pediatric patterns, and one built from urban hospitals may falter in rural clinics. The result is uneven care, lower trust, and real risk for patients and providers.
Expert tip. Start with coverage that mirrors your population and document who is included and who is not. Compare accuracy by age, sex, ethnicity, language, and care setting before launch and on a regular schedule after launch, with clear thresholds that trigger review. If gaps appear, add missing data or adjust the model, then re-test with clinicians.
Regulatory hurdles and compliance
High accuracy does not win approval on its own. Reviewers want the full story: the source and consent for the data, how you cleaned it, how you built and tested the model, and proof that the results hold up in real clinics. They also expect clear risk controls, audit trails, human oversight, and decisions that people can understand. If the system looks like a black box or the paperwork is thin, approval stalls.
Expert tip. Skip jargon and run a simple risk process that anyone can follow. List what could go wrong, who could get hurt, how likely it is, how severe it is, and how you could reduce that risk. Add checks to verify your controls work, record any residual risk, and update the file when the model or data changes. Treat privacy as design work, not a checkbox, with HIPAA and GDPR in mind.
Integration and adoption
AI fails when it sits outside the daily workflow. Clinicians do not have time to jump between screens or decode complex dashboards during a visit. If insights do not appear inside the EHR at the moment of care, adoption drops, and trust erodes.
Expert tip. Ensure compatibility with major EHR systems such as Epic, Cerner, and Meditech, and provide targeted training that positions generative AI in healthcare as an assistant, not a replacement. Also, keep clinicians in control of final decisions, and design clean, intuitive interfaces.
Shortage of machine learning experts
Healthcare needs AI talent faster than the market supplies it. Large tech firms hire many of the best people, so hospitals and startups struggle to staff projects and keep them on track. Progress slows, rollouts slip, and small internal teams carry too much load.
Expert tip: Train current staff in ML fundamentals and MLOps (model operations) — how to run, monitor, and update models safely. Pair that plan with a specialist partner, such as Relevant, to close skill gaps, accelerate delivery, and keep work aligned with clinical workflows and regulatory requirements from the FDA, EMA, HIPAA, and GDPR.
Our success case: AstraZeneca
AstraZeneca’s Medical Affairs teams had more CRM data than could realistically be reviewed. Decisions took longer, costs rose, and every step had to meet strict rules from the FDA, EMA, HIPAA, and GDPR. The team needed a safe way to find the signal in the noise without adding more manual work.
Relevant Software experts built an AI workspace that acts like an intelligent assistant for the CRM. It reads notes and records, spots patterns, and highlights what matters. The platform runs on Google Cloud and uses advanced language models, similar to ChatGPT, to understand text at scale.
Medical Science Liaisons open one screen and see a short summary, key trends by product and region, and suggested next steps. Outreach to healthcare professionals becomes timely and relevant, since each conversation starts with a clear context rather than guesswork.
Here is the impact in day-to-day work: teams save more than 20 hours a week on manual CRM review, market access costs drop by half, and decisions move through the pipeline faster, giving leaders earlier visibility into results.
Security and compliance remain the foundation. Data stays encrypted from end to end, access follows roles so only authorized staff see sensitive records, and an audit log records each action. The platform stays aligned with the FDA, EMA, HIPAA, and GDPR as usage grows.
15 future trends and innovations of ML in healthcare
Machine learning already shapes diagnostics, drug discovery, and hospital operations. The next wave brings tools that act faster, fit daily work, and meet strict safety rules. Here are the trends that matter and what they change.

1. Multimodal foundation models: New models read images, labs, notes, and signals together, producing one risk score and unified patient view that helps doctors catch patterns earlier and act faster.
2. On-device intelligence for medical hardware: Small models run on scanners, monitors, and wearables, so alerts arrive instantly with lower cloud cost and higher reliability.
3. Federated learning at scale: Hospitals train shared models while data stays local, which raises accuracy and preserves privacy and compliance.
4. Synthetic data: AI creates realistic, artificial patient data to fill rare cases, improve model balance, and strengthen validation without exposing sensitive or identifiable health information.
5. Digital twins of patients and organs: Virtual copies of patients or organs help clinicians test treatment options safely before real procedures, lowering risks and improving planning for complex interventions.
6. Causal ML for decisions, not predictions: These models show cause and effect rather than correlation, guiding therapy choices, doses, and timing, which leads to more precise, evidence-based medical decisions.
7. Faster clinical trials with real-world evidence: Machine learning finds eligible patients, flags risky sites, and predicts dropouts, helping sponsors run adaptive studies faster and bring safe drugs to market sooner.
8. Trust by design for clinicians: AI tools now show key factors behind each prediction with confidence levels and evidence links, building clinician trust and supporting regulatory acceptance.
9. Guardrails for AutoML and AI co-pilots: Automated ML tools include strict data contracts, policy checks, and feature stores to keep speed, safety, and auditability balanced throughout development and deployment.
10. Continuous monitoring: Bias dashboards and drift alerts track model behavior after launch, ensuring stable performance across hospitals and triggering retraining when accuracy begins to slip.
11. Stronger privacy technologies: Techniques like differential privacy, secure enclaves, and encrypted computation protect sensitive genomic and EHR data while still allowing advanced machine learning analysis.
12. Interoperability that finally works: FHIR-native apps and event streams connect EHRs, imaging systems, and devices, allowing ML tools to integrate easily and share data safely across healthcare settings.
13. Genomic and proteomic ML at the bedside: Faster gene and protein analysis supports precision medicine by helping clinicians choose the right treatment based on each patient’s biological profile.
14. Smarter NLP for clinical text: Language models read notes, radiology reports, and discharge summaries together, producing clear summaries and reducing errors caused by missing or inconsistent documentation.
15. Safety cases for AI as a medical device: New standards like GMLP and SaMD ensure AI medical tools include full evidence, clear oversight, and post-market monitoring for lasting patient safety.
Implement machine learning in healthcare with Relevant Software
At Relevant Software, we create AI solutions built around the real needs of healthcare, giving doctors clear insights, hospitals reliable and secure systems, and patients accurate care delivered exactly when it’s needed. Every product we deliver is built to be practical, trustworthy, and compliant from day one.

Our solutions are:
- Regulatory-ready. Developed with HIPAA, GDPR, and FDA standards in mind.
- Bias-free and explainable. Providing fair, transparent recommendations that clinicians can validate.
- Secure and scalable. Protected by federated learning and strong encryption for enterprise-level safety.
- EHR-compatible. Integrated with hospital IT systems for smooth, disruption-free adoption.
We work with hospitals, MedTech innovators, and biotech firms through healthcare development services that drive measurable results. From sharper diagnostics to streamlined workflows and better decision support, our solutions let healthcare professionals focus on their most important task — saving lives.
Partner with Relevant Software’s experts and hire AI engineers to bring machine learning into healthcare the right way, securely, ethically, and with proven impact. Contact us!

Hand-selected developers to fit your needs at scale! Let’s build a first-class custom product together.

