What is FHIR in Healthcare? A Practical Guide to FHIR APIs and Implementation

Healthcare data holds real value, but often sits in systems that cannot work together. FHIR unlocks that value by standardizing how records move and how apps connect. Before the rollout, one question matters: what is FHIR, and how do FHIR APIs make integration practical?
This FHIR implementation guide is written for providers and developers. It explains how FHIR works, where it delivers the most value, and a step-by-step path to implementation in real care. The guidance fits naturally within modern healthcare development services, programs, and governance.
from 25 countries outsourced software development to Relevant
We provide companies with senior tech talent and product development expertise to build world-class software.
What is FHIR in healthcare?
Picture this: You walk into any hospital today and witness a common frustration-data scattered across disconnected systems. Lab results in one system, prescriptions in another, and imaging files in yet another. Clinicians spend valuable time searching for information instead of caring for patients, leaving them to question why their medical records cannot simply follow them.
The industry has been engaged in a prolonged discussion on “interoperability,” a term that has often been hindered by outdated technology and rigid standards. It is in this challenging environment that the FHIR standard for healthcare has emerged as a crucial solution.
FHIR, or Fast Healthcare Interoperability Resources, is a standard created by HL7 that sets common rules for formatting and exchanging health data. Unlike older standards, it uses familiar web tools such as RESTful APIs, JSON or XML for data formats, and OAuth for access control. In practice, this lowers the barrier to adoption and makes integration far more realistic for hospitals, software vendors, and startups.
Technology turns these principles into real-world connections. Imagine a clinician who wants allergy information from an external EHR to appear instantly in their own system, or a mobile app that needs to pull blood glucose results into a patient dashboard. Instead of building custom bridges for every connection, developers can use the same API framework to move that data quickly and securely. It’s less about replacing systems and more about finally allowing them to cooperate.
One of the key advantages of FHIR in healthcare is its adaptability. It structures information into modular “Resources,” each representing a single element of a patient’s record, such as a medication, test result, or allergy. These FHIR Resources can operate independently or link together to form a complete history. This flexible structure allows organizations to integrate FHIR gradually, avoiding the need for a complete system overhaul. Hospitals can see more connected patient data, developers can deliver projects faster with less complexity, and patients can finally gain continuity of information, regardless of the provider they visit.
Benefits of implementing FHIR
Implementing Fast Healthcare Interoperability Resources (FHIR) lifts interoperability and reduces rework. With Relevant Software expertise in planning and testing, delivery stays consistent across releases.
- Interoperability that holds up. Systems use the same fields and codes, so interface errors drop.
- Faster clinical decisions. Medications, allergies, and vital signs appear in a single view, eliminating duplicates and delays.
- Lower integration cost. Teams rely on standard APIs and formats already known in health IT.
- Better patient experience. Portals and apps show the same information clinicians see.
- Research-ready data. A consistent structure supports cohort and outcomes studies with less data cleansing.
In short, FHIR streamlines operations, improves care, and lowers cost while strengthening the data foundation for analytics and research.
Now let’s move from the “why” to the “how.”
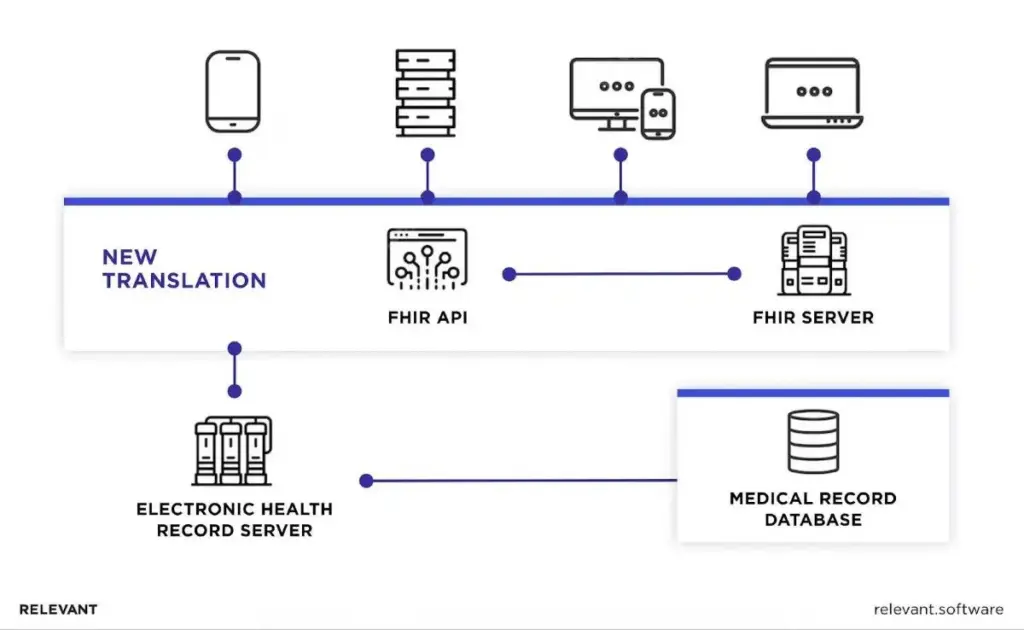
What is FHIR API?
That is a web interface that enables software to read or write health records conforming to the FHIR standard. It uses REST for requests, JSON or XML for formats, and OAuth for secure access. Many teams document endpoints with OpenAPI, but that is optional. The API is the practical layer of a FHIR framework: it powers real FHIR solutions and anchors FHIR development, enabling apps to connect, exchange the right fields, and display the same facts across systems.
How it works in an EHR scenario
- A patient app requests allergies and current medications for one person.
- The EHR’s FHIR endpoint authenticates the app, checks permissions, and returns only the requested Resources.
- A care-management tool requests the last 10 vital signs; the same API returns only those observations, with codes and units the tools agree on.
- A research pipeline pulls a defined set of de-identified records using bulk operations from the same server.
This focused, standards-based exchange lets portals, mobile apps, analytics platforms, and partner systems use the exact source of truth without custom one-off bridges. If you want background on the standard itself, start with our overview of HL7 standards and then explore SMART on FHIR for app launch and scopes within clinical workflows.
Your next read: Digital twin in healthcare
Key components of FHIR APIs
Let’s take a closer look at what lies behind the FHIR API standard and how it helps medical institutions ensure adaptability, coherence, and efficiency in managing healthcare information.
- Resources, often called building blocks, are the main structural components that store various types of information, such as clinical observations, medications, and patient details. You can combine these resources in different ways to meet your organization’s data model needs.
- Extensions allow you to adjust resources to fit unique healthcare use cases and your organization’s requirements. They help you add new properties or attributes to a resource that aren’t available in the base specification. So, you can tailor FHIR resources to align with your specific data structures and workflows.
- Profiles are guidelines that you can use on top of core specifications for resources and apply to a particular context. Specifically, as different countries, regions, and organizations have different legal requirements, they help customize data to meet those rules. As part of the FHIR API documentation, profiles also enable you to define additional operations, specify search parameters, and adapt to diverse healthcare scenarios.
How FHIR APIs work
Such variations, such as the Epic FHIR API and SMART on FHIR API, are similarly helpful for extracting large volumes of data from any healthcare system. Their functionality primarily depends on their structure, design principles, data formats, and communication protocols, which we’ll review below.
They have a well-defined structure and design principles that emphasize simplicity and efficiency. The structure is modular, consisting of resources that represent different types of healthcare data. Each resource is unique and can be easily adjusted to your specific healthcare data demands.
As for data formats, the FHIR framework supports XML and JSON, which are compatible with almost any system and technology. These formats are common languages for structured data models. As a result, APIs can integrate with numerous systems, whether you use legacy infrastructure or advanced technologies.
Another advantage is that they employ RESTful communication protocols for system interaction. These protocols serve as standards for creating, reading, updating, and deleting resources in modern technologies, thereby simplifying adherence to standards when managing and exchanging data.
The most common approaches to FHIR API implementation
Implementing FHIR improves healthcare communication and data exchange. Cloud options such as the Azure FHIR API and Cerner FHIR API show how fast teams can stand up compliant endpoints and scale without heavy infrastructure work.
The FHIR standard is grounded in a clear FHIR data model. It defines how information is stored, retrieved, and shared, which directly affects the success of any FHIR API implementation. Well-structured Resources, stable identifiers, and consistent codes lead to cleaner results and fewer rework cycles.
These models also define the structure and connections that enable FHIR-based APIs. When properly configured, applications share accurate data within the correct context, support clinical review, and minimize errors. In regulated environments, which are typical for pharmaceutical software development services, teams depend on validation-friendly practices that ensure clear traceability, audit trails, and documented testing evidence.
The most common approaches to implementation:
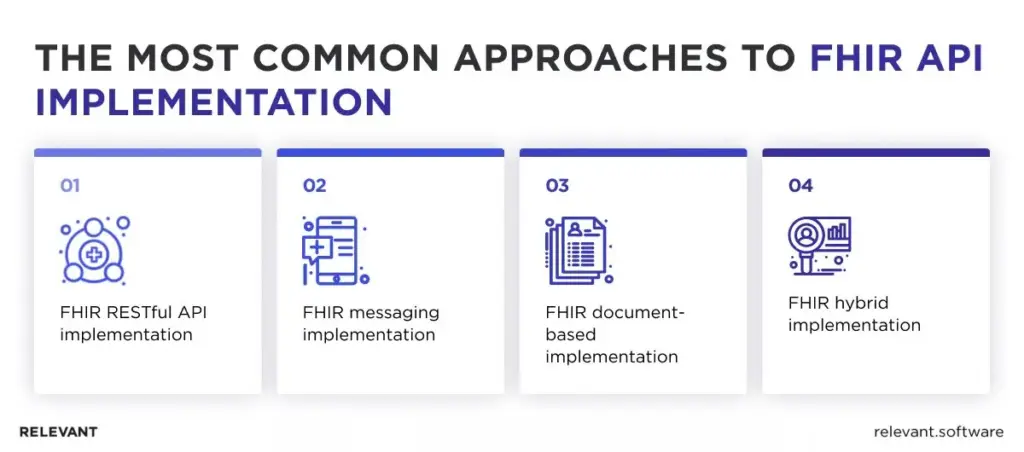
1. FHIR RESTful API implementation
In a RESTful API implementation, FHIR leverages web standards to create, read, update, and delete (CRUD) operations on resources. This approach is particularly valuable in real-time applications where healthcare systems need to interact dynamically. It’s a straightforward method in which resources are treated as URLs and standard HTTP verbs are used. RESTful API implementation is widespread because of its simplicity, scalability, and compatibility with modern web architectures.
RESTful principles
Many apps, whether on mobile devices or web browsers, use REST (Representational State Transfer) as the basis for their APIs, and FHIR is no exception. REST’s main feature is to ensure every interaction between the client and the server is complete, containing all the necessary information for the request. Any data exchange that uses REST is considered RESTful.
Healthcare FHIR also uses this REST standard for data exchange, and one of its advantages is its lightweight interfaces, which speed up data transmission and processing. A RESTful resource provides a way to access data through specific endpoints, structures, and formats. The more precisely you define these elements, 687uthe more accurate the data exchanges are. For instance, a third-party healthcare app, such as a Patient’s Portal, can access patient data from an EHR system via an API. What you need to do is submit a request specifying the type and amount of data you require from the EHR server.
CRUD operations in FHIR
CRUD stands for the four fundamental operations—Create, Read, Update, and Delete—used to interact with FHIR resources. Understanding them is key to working with APIs because they let you actually manipulate and perform specific actions on data. So, they mean adding new data (Create), retrieving existing data (Read), modifying stored data (Update), and removing unnecessary data (Delete) within a system.
CRUD operations support the healthcare system’s responsiveness and adaptability while helping you keep data accurate, up-to-date, and structured. They also offer a user-friendly interface that makes interaction with the system easier, improving the overall user experience and workflow.
2. FHIR messaging implementation
In the messaging implementation, FHIR resources are used within existing HL7 message structures. That enables healthcare systems to leverage FHIR’s granularity and flexibility while maintaining their investment in HL7 messaging infrastructure. It’s an event-driven model in which a trigger event in one system sends a message to another system. This approach is suitable for batch-style and background processing tasks.
3. FHIR document-based implementation
In the document-based implementation, FHIR resources are bundled into self-contained, discrete units of healthcare information called documents. That is a particularly effective way to handle complex use cases that involve multiple resources, such as a discharge summary or a referral note. These documents can then be readily shared, stored, and retrieved, making them ideal for interoperability purposes.
4. FHIR hybrid implementation
As the name suggests, a hybrid implementation combines various approaches tailored to the healthcare system’s needs. For example, a healthcare provider could leverage a RESTful API to facilitate real-time interactions, use messaging for batch processing, and employ document-based approaches for handling complex FHIR use cases. This flexible approach ensures that healthcare systems can leverage FHIR platform strengths in ways that best suit their operational needs and strategic goals.
Choosing the right approach for FHIR implementation requires a careful understanding of the healthcare system’s requirements, existing infrastructure, and strategic goals. With the right approach, FHIR can significantly enhance healthcare data interoperability, leading to improved patient care and operational efficiency.
FHIR implementation: step-by-step guide
Implementing FHIR works best when the plan remains clear, the scope remains focused, and every team member understands the expected outcome. If you want expert support from start to scale, our HL7 FHIR services cover strategy, profiling, server setup, and integration.
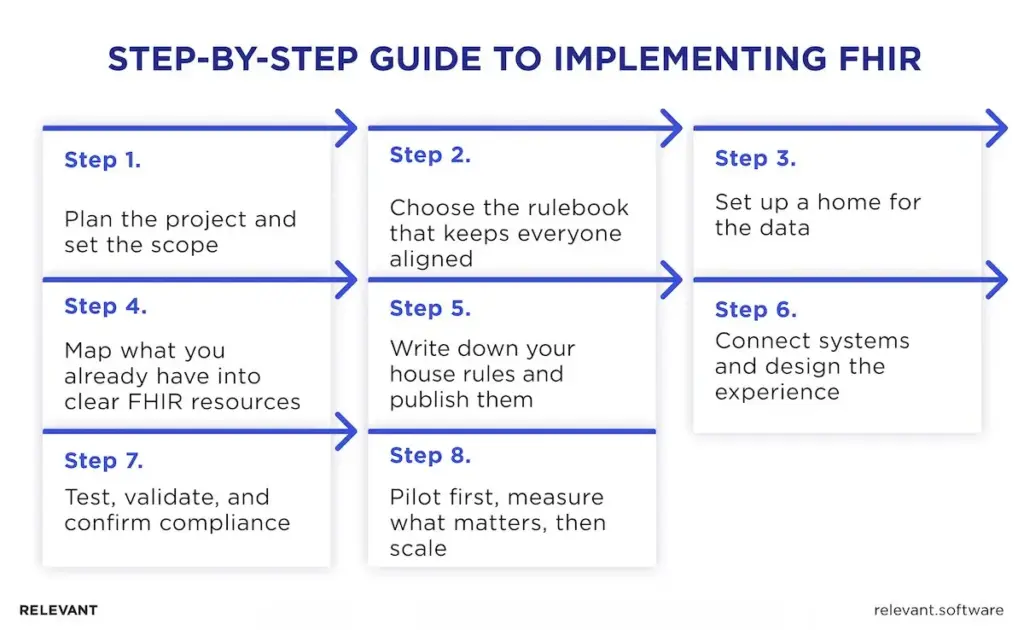
1) Plan the project and set the scope
Define two or three outcomes that matter to care and operations. Faster data exchange, a single medication list in the electronic health records, or a reliable view of vital signs across sites are good starting points—name stakeholders in clinical, privacy, IT, and finance. Set a timeline that includes discovery, pilot, and rollout. Record obvious risks of FHIR integration, such as identity matching, code sets, and privacy controls, and decide in advance who resolves each one.
2) Choose the rulebook that keeps everyone aligned
Adopt FHIR US Core as your baseline because it lists required fields and code systems for common data. That prevents rework later and supports healthcare interoperability across partners. Use US Core to decide what a Patient, an Allergy, or an Observation must contain, so every system reads the same structure and produces quality data.
3) Set up a home for the data
Deploy a FHIR Server that acts like a secure library for your records. It stores data in a consistent format, controls who can see what, and provides a single front door for data exchange with portals, EHR modules, and analytics tools. That reduces dependence on point-to-point pipes that often break inside legacy health environments.
4) Map what you already have into clear FHIR resources
List the fields that matter for your first outcome and match them to FHIR terms. Blood pressure, heart rate, and temperature belong in Observation resources, so your team can search and display vital signs without confusion. Link each Observation to the right Patient and encounter. This simple act improves context for clinicians and provides patients with a clear timeline at home.
5) Write down your house rules and publish them
Your program will adopt local decisions that go beyond US Core. Capture those decisions in short examples and plain rules, then publish them with the FHIR IG Publisher as a small, readable site. Everyone now works from a single source of truth, reducing uncertainty and speeding approvals. Treat this guide as part of the product, not an afterthought.
6) Connect systems and design the experience
Use the API to move data between the electronic health records, the patient portal, and any medical applications that support care. Keep screens straightforward, with one clear view for a clinician and the same values for a patient. When you feed consistent data to clinical decision support, alerts fire at the right time and in the right place, which improves confidence at the bedside.
7) Test, validate, and confirm compliance
Check that each record meets your US Core rules and your local guide. Verify that search results show the correct patient, the correct date, and the correct units. Confirm privacy controls and audit logs. Run short drills where a nurse, a physician, and a patient complete everyday tasks, then capture issues and resolve them before rollout.
8) Pilot first, measure what matters, then scale
Run a time-boxed pilot in one clinic or one service line. Track how long it takes to find key data, how many duplicate orders appear, and whether portal use rises. If results meet targets, add the next data set. Medications and allergies usually follow vital signs, then labs, then problems, on the same server, with the same guide and the same discipline.
FHIR implementation example
A hospital wants a single trusted view of bedside measurements across wards and the portal. The team picks a national guide to lock in the right fields and codes, sets up a secure data service to store and search records, maps blood pressure and pulse as standard measurements linked to each person’s chart, and publishes a short online guide with clear examples for staff and vendors. Nurses see the latest numbers in one place, patients see the exact figures at home, and leaders can measure better data flow and smoother care coordination without replacing core systems.
FHIR implementation challenges
Rolling out FHIR brings clear benefits, yet several hurdles can slow progress if you ignore them. Here are the issues we see most often with Relevant Software clients, along with how teams address them.
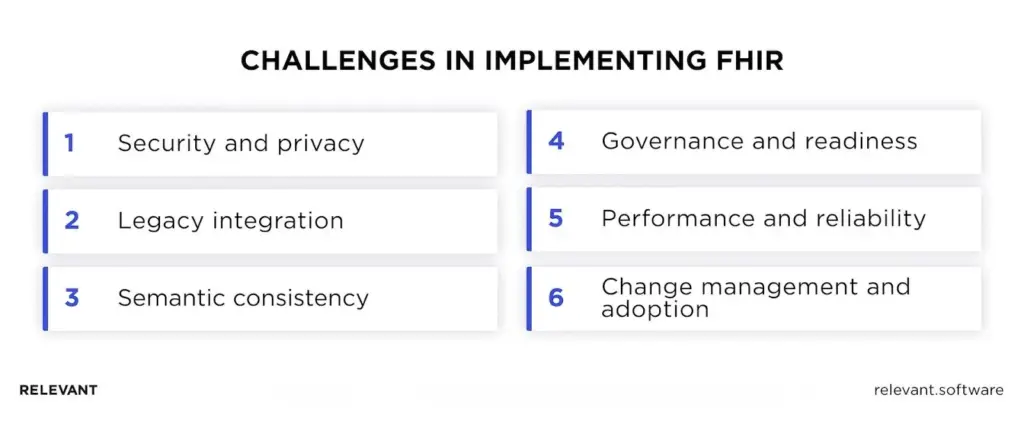
Security and privacy
Data moves farther and faster with FHIR, which widens exposure. Successful programs rely on strong authentication, role-based access, encryption, explicit consent handling, and routine audit reviews to keep access appropriate.
Legacy integration
Older systems use custom codes and identifiers that do not align with modern models. Teams that succeed map these differences with real samples, settle on a single matching strategy, and keep batch jobs from clashing with near-real-time updates.
Semantic consistency
FHIR defines structure, while local meaning can still vary. Mature rollouts anchor on a jurisdictional guide like US Core, publish local rules with examples, and validate records against those rules across environments.
Governance and readiness
Interoperability changes who owns decisions and how work flows. Programs that maintain momentum have named owners for product, clinical, privacy, and integration choices, a regular forum for decisions, and training built around everyday clinical tasks.
Performance and reliability
Trust depends on fast, predictable responses. Stable services keep payloads reasonable, separate interactive reads from bulk movement, and watch latency and error rates so issues surface before users notice.
Change management and adoption
An API alone does not change care. The services that stick present the most relevant facts on a single clinician screen, mirror those details in the patient portal, and tune alerts with clinical leaders based on real usage and outcomes.
FHIR vs HL7: complementary or replacement?
Short answer: They work together. HL7 v2 and v3 still power the main data pipelines in many hospitals, while FHIR introduces a modern approach for accessing and exchanging smaller data segments via web APIs.
For a straightforward comparison, check out FHIR vs HL7.
What HL7 v2 and v3 do well
HL7 v2 messages work like quick system-to-system updates — notifying when a patient checks in, a lab test begins, or results are ready. They’re fast and handle large volumes efficiently. HL7 v3 and CDA, on the other hand, deal with complete documents, such as discharge summaries, that must remain intact for recordkeeping. These standards are reliable and widely used, but can be challenging to modify and often differ across vendors.
What FHIR adds
FHIR treats data as small, well-defined pieces that applications can request on demand through an API. A care app can ask for only allergies or recent vital signs. A portal can show a clean medication list without pulling an entire chart. Search works well. Access control can target only the fields a role needs.
How to use them together
Keep v2 where message traffic already meets clinical needs. Keep CDA documents so that a legal snapshot can move as a whole. Add FHIR support for patient and clinician apps, partner connections, analytics, and decision support that require precise queries and near-real-time views.
When to consider a shift
Move an interface to FHIR when the team needs faster partner onboarding, more explicit data rules, or finer-grained control over who sees what. Keep the rest on v2 or CDA until a clear benefit appears. This approach avoids big rewrites and still raises interoperability step by step.
Bottom line
FHIR offers a realistic path to true interoperability, improved patient outcomes, and more efficient operations. The process isn’t simple, but with a clear plan, well-defined scope, and commitment to best practices, the results become tangible and lasting.
If this is your first program of this size, the task can feel heavy. You can hand it to a partner with a record of safe delivery. Relevant Software experts focus on healthcare data exchange and HL7 adoption, with a special focus on FHIR.
Our team can:
- Advise as a part of healthcare IT consultation on a path to FHIR-based interoperability after a structured review of your current systems.
- Augment your staff with engineers who handle configuration, integration, data quality, and performance tuning.
- Provide a dedicated team that designs and builds interoperable solutions from the ground up.
If you want expert help from discovery to rollout, explore our HL7 FHIR services for healthcare companies or contact us to discuss your timeline and goals.
FAQ
What is interoperability in healthcare exactly?
Interoperability in healthcare refers to the seamless exchange of healthcare data among systems, organizations, and stakeholders. It involves the ability of diverse healthcare systems, such as electronic health records (EHRs), clinical and laboratory systems, and medical devices, to communicate, interpret, and effectively use shared data.What are the benefits of using FHIR for sharing medical charts?
FHIR enables the seamless, standardized sharing of medical records among healthcare providers, patients, and other stakeholders. That enhances care coordination, supports informed clinical decision-making, and fosters patient engagement in their health management.How can organizations explore FHIR resources for implementation guidance?
Organizations can leverage the HL7 FHIR website, which offers a wealth of resources, including detailed technical specifications, use case examples, and implementation guides. There are also community forums and educational events for learning and networking opportunities.How does FHIR enable collaborative access to personal health records?
FHIR facilitates collaborative access to personal health records by standardizing the structure and exchange of data. It enables different healthcare systems to understand and use the data, allowing various providers to contribute to and access a patient’s health record, fostering collaborative care.What is the FHIR API, and what is a simplified data model?
That is a modern standard for online healthcare data exchange that simplifies data models to help your organization achieve interoperability. It brings standardization, strengthens security, and ensures that patient information is accurate, accessible, and easily shareable between the systems. FHIR-compliant solutions improve clinical decisions and help doctors deliver personalized patient care.How to test FHIR API?
When you test an API, you should check the structure of its resources and how it responds to different requests. During testing, you can identify and fix issues to strengthen the API’s performance, functionality, and overall stability. Thorough API testing helps avoid unpleasant surprises during implementation, ensures your solution meets industry standards, and enables the reliable and secure sharing of healthcare information.How does FHIR API ensure data security?
First, it uses strong authentication methods to confirm user identity and permissions before providing access to sensitive healthcare information. Second, they use secure communication protocols, meaning the data transferred between health apps remains encrypted and protected from unauthorized access. Such strong security measures can help you build patients’ trust and maintain confidentiality while complying with strict healthcare regulations.What are the key components of an FHIR API request?
A typical request should include the following elements: u003cbru003eu003cbru003eEndpoints to define the server and type of resource;u003cbru003eMethods to indicate the action you want to perform; u003cbru003eHeaders to provide meta and additional data; u003cbru003eRequest body that contains the actual data. u003cbru003eu003cbru003eTogether, these components make up an API request that retrieves data from another source, such as the EHR system of a clinic the patient previously visited, and makes it accessible within your own EHR system.What types of data can FHIR manage?
They’re pretty versatile and can handle practically any healthcare data. We’re talking about clinical, administrative, and infrastructural data, encompassing patient records, medication information, diagnostic reports, and more. That’s why they are a top choice for healthcare solutions that require accurate healthcare information accessible in a few clicks.

Hand-selected developers to fit your needs at scale! Let’s build a first-class custom product together.

